Dear Editor,
Infantile haemangioma of the lip is a therapeutically challenging vascular tumour, given the occurrence of local complications and the long-term risk of a cosmetically unesthetic lip contour. Instituting early medical management with beta-blockers is important, but often these patients have incomplete involution with a residual lip deformity.1 We report a case of a young girl with a mixed infantile haemangioma of the upper lip, which showed near complete restoration of normal lip contour with intralesional radiofrequency followed by lip reduction surgery [Video 1].
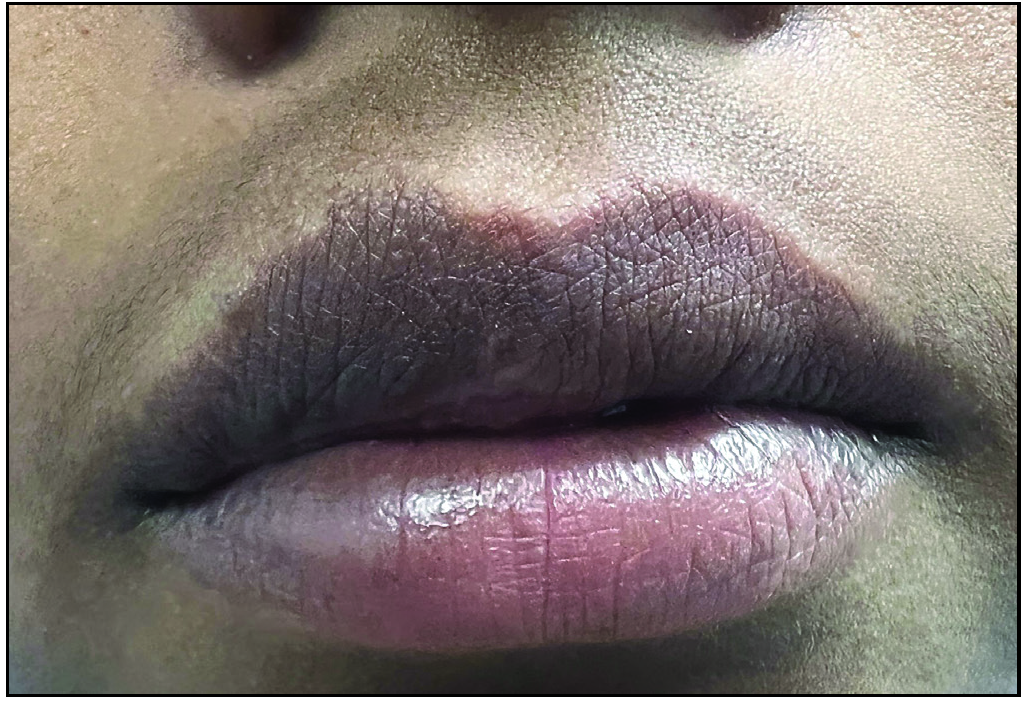
Video 1: Intra-operative procedure of intra-lesional radiofrequency ablation followed by lip reduction surgery for infantile hemangioma.An 11-year-old girl presented to us with a soft, compressible, dusky, erythematous swelling involving the right side of the upper lip since birth [Figure 1a]. The swelling was non-tender with a slight increase in local temperature with no palpable thrill or bruit on auscultation. The child has received oral propranolol for about six months at five years of age with minimal reduction in swelling. The swelling caused significant lip deformity, with the right side of the upper lip protruding beyond the left half and distorting the philtrum and the smooth vermilion border. The child hesitated to attend school, and her parents were very anxious.

Export to PPT
We initially planned serial sessions of intralesional radiofrequency ablation, as first described by Subhadarshani et al.2 After cleaning and draping, the right side of the upper lip was infiltrated with local anaesthesia (2% w/v lidocaine with epinephrine), starting from the right commissure and progressing medially. The anaesthesia was infiltrated parallel to the vermilion border and into the bulk of the swelling, carefully withdrawing the plunger each time before injecting. Thereafter, a small window was created in the proximal end of the plastic sheath of an 18-G intravenous cannula with a surgical blade inserted into the tissue bulk. A pointed radiofrequency probe set at 20 mW power in coagulation mode was connected to the metallic cannula through the window. The cannula was then moved in different directions, coagulating the tumour tissue. Careful consideration was given to avoid touching the cannula to the labial mucosa at the point of entry to prevent superficial scarring. Postoperatively, the patient was advised analgesics and a topical antibiotic at the point of entry.
The patient underwent six sessions of intralesional radiofrequency coagulation over a period of 1 year with about a 50% reduction in the size of swelling [Figure 1b]. However, there was minimal improvement in the last two sessions, and the lip contour was still distorted. We now proceeded with lip reduction surgery to improve the aesthetic outcome further.
Export to PPT
Using an indelible marker, the area to be excised was marked before infiltration anaesthesia. Thereafter, using a 15-number surgical blade, a 3:1 elliptical excision was made, with the width of the excision corresponding to the extent of excess tissue. The amount of tissue bulk to be removed was carefully decided intra-operatively, balancing the ease of wound closure under minimal tension without leaving any extra redundant tissue. Intraoperative haemostasis was achieved using a bipolar radiofrequency probe to coagulate any bleeders during exploration. The labial mucosa was closed in 2 layers with a buried sub-cutaneous suture with 4-0 vicryl and surface approximation with 5-0 prolene. Postoperatively, she was advised to take oral painkillers and antibiotics. A week later, the surgical site had healed, and the sutures were removed, though some postoperative oedema still existed.
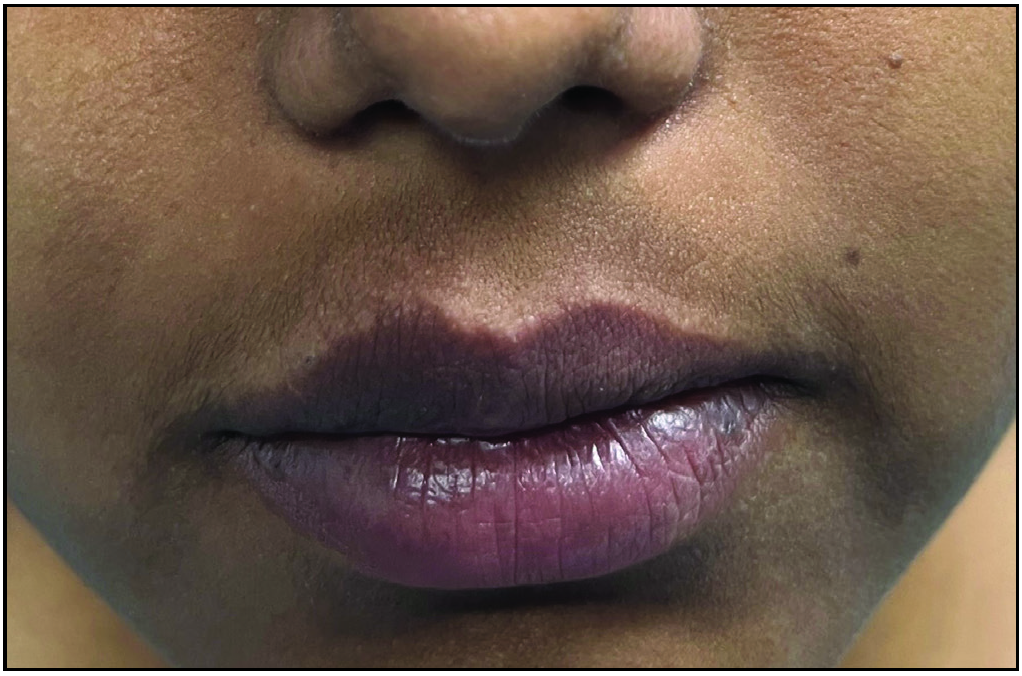
At 1-month follow-up, the swelling was remarkably reduced, which was now barely perceptible. The upper lip contour had been restored, and so had the philtrum with a smooth curved vermilion border [Figure 1c]. Besides a marked objective improvement compared to previous photographs, the patient and her parents were highly satisfied with the surgical outcome.
Export to PPT
Hemangiomas are benign vascular tumours with a self-involuting phase, such that 70% completely regress by seven years of age. When these occur on the lips, they are notorious for causing functional and cosmetic complications, the most important being ulceration during the proliferative phase and residual lip deformity during the involutional phase. A retrospective study by Cawthorn et al. highlighted that a lip contour defect occurred in 26.5% of haemangiomas involving the lip, especially those with a deeper component and the vermillion border.3 While oral propranolol leads to the involution of the haemangioma, a deep component often results in substantial residual bulk, necessitating surgical intervention. Our patient also had a mixed hemangioma (with a deeper component), crossing the vermilion border and hence was prone to cosmetic deformity.
There is no consensus on the optimal age of operative intervention for lip haemangiomas. Some authors believe that early intervention in the proliferative phase is beneficial,4 while others contest that delaying the surgery allows self-involution of the haemangioma.5 Our patient had presented around puberty and was then taken up for surgical intervention. Various surgical modalities have been used in lip hemangiomas, including radiofrequency ablation, debulking, intralesional sclerotherapy and carbon dioxide laser ablation.6–8 In our approach, the initial application of radiofrequency ablation not only helped decrease the tissue volume, facilitating easy surgical debulking thereafter but also helped achieve better haemostasis because of the coagulation of feeder vessels. Narayanan et al. used a similar technique to treat port wine stain-related lip hypertrophy.9
Radiofrequency ablation is effective and safe for treating small to moderate-sized lip hemangiomas. Lip reduction is a complementary technique that can then be used to remove any residual hemangioma tissue and improve the cosmetic outcome. Combining these techniques can result in a successful treatment outcome with minimal cosmetic morbidity and scarring.
留言 (0)