Psoriasis is a common, chronic inflammatory disorder, known to affect skin, nails, and joints with a worldwide prevalence of 2–3%.1 Nail psoriasis is associated with significant functional impairment and psychological handicap, leading to an altered quality of life. However, we are yet short of effective treatment modalities for nail disease. Various inflammatory cytokines including tumour necrosis factor (TNF-α) and interleukin-17 (IL-17), IL-12, IL-23, and IL-6 play an important role in the pathogenesis of psoriasis, but their role in the pathogenesis of nail psoriasis remains largely underexplored. These cytokines are also important drug targets and are used in the treatment of severe psoriasis; however, their relation with nail disease needs comprehensive evaluation. This can help us decide on effective treatment options for nail disease.
Nail psoriasis seems to be a surrogate marker for psoriatic arthritis. It could, in fact, be the link between psoriasis (nail involvement seen in 10–78% cases) and psoriatic arthritis (nail involvement seen in 70–80% cases).1 We are beginning to realise the similarities and differences between psoriasis and psoriatic arthritis and nail psoriasis becomes an important terrain to explore. We conducted this study to evaluate the serum levels of inflammatory cytokines and biomarkers in patients with nail psoriasis as compared to psoriasis patients without nail involvement and healthy controls.
MethodsA cross-sectional study of patients presenting with psoriasis, with and without nail involvement, was carried out in a tertiary-level teaching hospital. The study protocol was approved by the Institutional Ethical Committee (IEC-HR/2019/41/34). Adult patients presenting with nail psoriasis (Group-I, n = 30) and without nail involvement (Group-II, n = 30) were sequentially recruited. Non-psoriatic otherwise healthy subjects attending dermatology OPD for unrelated minor illnesses, which are not likely to affect serum cytokine levels (Group-III, n = 20) were included as controls. An informed written consent was obtained from all participants. Patients with psoriatic erythroderma, cardiovascular disease, any acute or chronic infections, and those on any form of systemic therapy for psoriasis for the past 1 month were excluded from the study.
The sample size was estimated based on a previous published study, evaluating serum levels of inflammatory cytokines in Greek psoriasis patients with nail involvement.2 This study estimated mean serum TNF-α levels to be 5.40 ± 1.17 pg/mL and 3.80 ± 1.63 pg/mL in psoriasis patients with nail involvement and without nail involvement, respectively. Keeping the Type I error at 5% and power of study at 90%, a sample size of 18 each in Group I and Group II was calculated (G Power ver3.1.9.2 for Windows).2 Rounding off the figures, we recruited 30 participants each in Group I and Group II and 20 participants in Group III [Table 1].
Table 1: Clinical profile of psoriasis patients (n = 60)
Patient Characteristics Study participants Group-I+ Group-II (n = 60) [Psoriasis] Group-I (n = 30) [Psoriasis with nail involvement] Group-II (n = 30) [Psoriasis without nail involvement] P-value (Group-I vs group-II) Male (n, %) 41 (68.33%) 22 (73.33%) 19 (63.33%) 0.406 Female (n, %) 19 (31.66%) 8 (26.67%) 11 (36.67%) Age (years) 36.83 ± 12.75 40.6 ± 12.6 33 ± 11.7 0.017*Mean ± SD
Median (min–max)
35 (18–60) 41 (18–60) 30 (18–60) Disease duration (years) 7.75 ± 9.87 9.9 ± 9.1 5.62 ± 10.13 0.0002*Mean ± SD
Median (min–max)
5 (0.08–40) 7.50 (1–40) 1.50 (0.08–40)Family history:
(n, %)
6 (10%) 4 (13%) 2 (6.66%) 0.389 Clinical types of psoriasis Plaque psoriasis 58 (96.66%) 28 (93.33%) 30 (100%) 0.491 Guttate psoriasis 12 (20%) 3 (10%) 9 (30%) 0.104 Scalp psoriasis 42 (70%) 20 (66.67%) 22 (73.33%) 0.573Psoriatic arthritis
(n, %)
4 (6.66%) 4 (13.33%) 0 0.038* PASI Score 10.24 ± 9.12 11.99 ± 11.41 8.48 ± 5.46 0.275Mean ± SD
Median (min–max)
7 (0–50.8) 10 (0–50.8) 6.50 (2–21.6) NAPSI score - 47.1 ± 29.62 - -Mean ± SD
Median (min–max)
36 (12–120)A detailed history and complete mucocutaneous examination were conducted and documented for all patients. Cutaneous disease severity and severity of nail disease were calculated using the Psoriasis Area Severity Index (PASI) and Nail Psoriasis Severity Index (NAPSI), respectively. All these patients were also assessed for joint involvement based on Classification of Psoriatic Arthritis (CASPAR) criteria.3
Thereafter, blood samples were drawn from all study participants for the estimation of serum TNF-α and IL-17, erythrocyte sedimentation rate (ESR), rheumatoid factor (RA factor), and anti-cyclic citrullinated peptide antibody (Anti-CCP). For serological assessment of IL-17, TNF-, and anti-CCP levels, 3–5 mL of peripheral venous blood was collected following aseptic precautions. This blood sample was centrifuged; serum was separated, stored at −20°C, and tested with commercially available enzyme-linked immunosorbent assay (ELISA) kits based on sandwich enzyme-linked immunosorbent assay technology [Table 2].
Table 2: Serological profile of study participants (n = 80).
Patient Characteristics
(n, %)
Study participants Group-I + Group-II (n = 60) [Psoriasis] Group-I (n = 30) [Psoriasis with nail involvement] Group-II (n = 30) [Psoriasis without nail involvement] Group-III (n = 20) [Healthy, non-psoriatic controls] Raised ESR [Males:>15 mm/h Female:>20 mm/h] 35 (58.33%) 24 (80%) 11 (36.66%) 1 (5%) RA factor [RF-Latex kit (Recombigen, Delhi, India)] 2 (3.33%) 1 (3.33%) 1 (3.33%) 0 Anti-CCP [C-peptide ELISA (CALBIOTECH, USA)] 2 (3.33%) 1 (3.33% ) 1 (3.33%) 0 TNF-α (pg/mL) [Human TNF Alpha ELISA Kit PicoKineTM (BOSTER BIOTECH, sensitivity: 9.375pg/mL)] Detected in 3 patients Detected in 1 patient Detected in 2 patients Not detected Mean IL-17 (pg/mL) [Human IL-17A ELISA Kit PicoKineTM (BOSTER BIOTECH, USA, sensitivity: 18.75pg/mL] [Mean ± SD Min- Max] 70.65 ± 183.22 113.39 ± 251.30 27.91 ± 18.22 25.67 ± 12.08 0–1298.37 9.37–1298.37 0–82.18 12.93–52.56The data collected were entered in MS Excel and analysed using SPSS (Statistical Package for the Social Sciences) software v20.0. Statistical analysis comprised calculating means and proportions. Appropriate statistical tests of significance including Mann–Whitney-U test (to compare median value for age, disease duration, and PASI), Chi-square test, Fisher Exact test, and Kruskal–Wallis test (to compare means of IL-17 among three groups) were applied to evaluate the statistical significance of differences between the study groups. A p-value of less than 0.05 was considered as significant.
ResultsThe median age was significantly higher for Group I patients as compared to Group II patients (p = 0.017) [Mann–Whitney-U test]. Group III was comparable with a median age of 37.5 ± 11.90 years and a male-to-female ratio of 1.5:1. The median duration of disease in Group I was significantly higher (p = 0.0002) than in Group II [Table 1]. The median PASI was higher in Group I compared to Group II; however, the difference was not found to be statistically significant (p = 0.275). In addition, 4/30 (13.33%) Group-I patients had concomitant arthritis while none of the Group-II patients had psoriatic arthritis. The total number of clinically involved nails was 465/600. The number of involved nails per patient ranged from 7 to 20 with a mean of 15.5 ± 4.07 per patient. The mean NAPSI was 47.1 ± 29.62 [Table 1].
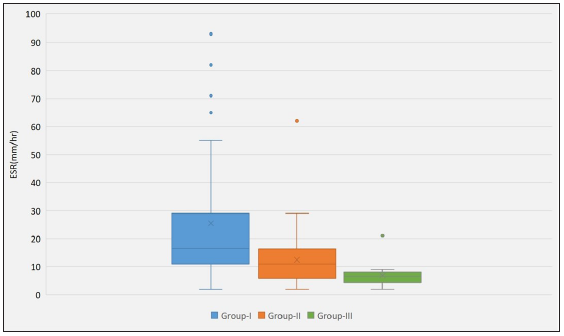
Only one patient of Group I and two patients of Group II had detectable TNF-α levels [Table 2]. As the TNF-α levels were below 9.375pg/mL (sensitivity of the assay kit) in the rest of the samples, mean values could not be obtained and comparison could not be done. The mean serum level of IL-17 was significantly higher for Group I when compared to Group II (p = 0.002) and Group III (p = 0.005) [Kruskal–Wallis test] [Tables 2 and 3, Figure 1]. The mean serum levels of IL-17 in Group II were higher than the controls, but the difference was not statistically significant (p = 0.938). The correlation between the Nail Psoriasis Severity Index (NAPSI) and serum IL-17 was found to be weakly positive (Spearman’s test; Rho = 0.355, p = 0.054). There was no correlation between serum levels of IL-17 and PASI in Group I patients (Spearman’s test; Rho = 0.13, p = 0.944). However, there was a strong negative correlation between IL-17 levels and PASI in Group-II patients (Spearman’s test; Rho = –0.368, p = 0.045). A raised ESR was found significantly more commonly in Group I than in Group II patients [Tables 2 and 3, Figure 2].
Table 3: Comparative evaluation of serological profile between three groups
Comparison between groups Raised ESR RA factor positivity Anti-CCP positivity TNF-α IL-17 Group I vs Group III 0.00001* 1 1 - 0.005* Group II vs Group III 0.016* 1 1 - 0.938 Group I vs Group II 0.0006* 1 1 - 0.002*
Export to PPT
Export to PPT
DiscussionThe pathogenesis of psoriasis is complex and incompletely understood. A strong interplay of genetic, environmental, and immune factors are known to be operative. The immunopathogenesis of psoriasis is driven mainly by T-lymphocytes and dendritic cells and maintained by a network of inflammatory cytokines, comprising mainly of the IL-23/Th-17 pathway.4 Cytokines including TNF-α, IL-17, and IL-6 play a critical role in promoting systemic inflammation. IL-12 and 23, released by dendritic cells, activate Th-1 and Th-2 to produce IL-17, IFN-γ, TNF-α and IL-22. These further directly stimulate keratinocytes to produce psoriatic lesions.5 With our increasing understanding of its complex immunology, targeted therapy has found an important place in psoriasis management. However, there is a paucity of studies evaluating immunological aspects of nail psoriasis, even though biologics targeting IL-17 and TNF-α have been found to be clinically effective.5
In literature, many studies have documented higher serum TNF-α in patients with psoriasis compared with healthy controls.6-9 However, our patients and controls did not show detectable serum TNF-α (9.375pg/mL being the detection limit of the assay kit used). A similar study by Gomi et al.10 reported elevated TNF-α levels in 6/21 psoriasis patients while none of the controls had detectable TNF-α level. Tigalonova et al.11 and Jacob et al.12 reported no significant differences in serum TNF-α levels between psoriasis patients and healthy controls. Saulite et al.13 reported an increased expression of TNF-α in psoriatic nails. TNF-α has also been found to be raised in psoriasis skin lesions even when serum levels are normal. Based on our study, it is difficult to draw conclusive inferences regarding serum TNF-α levels in patients with nail psoriasis.
A number of studies have documented increased serum IL-17 in plaque psoriasis patients as compared to healthy controls.5,7,14 We found significantly higher serum IL-17 levels in psoriasis patients with nail involvement as compared to those without nail involvement (p = 0.002). These values were higher than those in the reference study by Kyriakou et al.2 This could be due to the inclusion of more severe cases in our series, including patients with concomitant PsA, and higher NAPSI and PASI scores. Our study highlights the elevated serum levels of IL-17 in patients with nail psoriasis, which could influence the decision regarding treatment options for the same.
A weak positive correlation between NAPSI and serum IL-17 levels was seen (Spearman’s rank test; Rho = 0.056, p = 0.806) while Kyriakou A et al.2 reported no such correlation. There was no correlation between serum levels of IL-17 and PASI in Group-I patients, whereas a strong negative correlation was seen between IL-17 levels and PASI in Group-II patients. However, most studies5 have reported a positive correlation between PASI and serum IL-17, while Takahashi et al.7 and Kyriakou A et al.8 found no correlation. This could be because tissue inflammatory cytokines levels may not always reflect in blood and vice-versa. In addition, whether the change in serum cytokine levels of psoriatic patients is the cause or consequence of the disease needs to be explored further. To the best of our knowledge, no available study has assessed serum TNF-α and IL-17 in nail psoriasis, except the reference study.2 The lack of conclusive studies and incomplete understanding of the exact pathogenesis of nail psoriasis highlights the fact that further work is needed.
LimitationsThe major limitation of our study was a small sample size. Also, meaningful analysis of the serum TNF-α could not be done between groups due to the low sensitivity of the TNF-α assay kit used. Other cytokines (IL-12/23, IL-6) could not be evaluated due to cost constraints. Age and sex matching between the groups could not be done.
ConclusionBased on our findings, we conclude that elevated serum IL-17 levels in psoriasis patients with nail involvement possibly suggests an important role in the pathogenesis of nail psoriasis. This may serve as a guide towards appropriate drug selection or monitoring of treatment response in nail psoriasis patients. However, further controlled studies involving larger sample size can help draw conclusive evidence.
Comments (0)