Inferior vena cava (IVC) injury is a severe vascular injury that can be classified as either iatrogenic or traumatic. Iatrogenic causes include endothelial damage due to venous catheter placement or IVC filter placement, as well as surgical complications associated with liver surgery.[1] Traumatic causes account for most IVC injuries, with 70–90% due to penetrating trauma and 10–30% due to blunt trauma.[2] The overall mortality rate for IVC injuries ranges from 34% to 70%.[3] Blunt traumatic IVC injuries are challenging to diagnose due to their nonspecific clinical presentation and the possibility of no extravasation of contrast medium on contrast-enhanced computed tomography (CT) despite the presence of a retroperitoneal hematoma.[4] Surgical management is a primary treatment approach; however, surgical access to the high-flow, low-pressure venous system can be challenging.[5] Endovascular treatment using stent grafts has been proposed as an alternative.[6,7] Non-operative conservative management has also been reported in hemodynamically stable patients without active bleeding.[8] However, reports of successful non-operative conservative management remain limited. We report a case of blunt traumatic IVC injury with bowel perforation and spinal cord injury. While the bowel perforation required surgical intervention, the IVC and spinal cord injuries were successfully managed conservatively, and the patient made a favorable recovery.
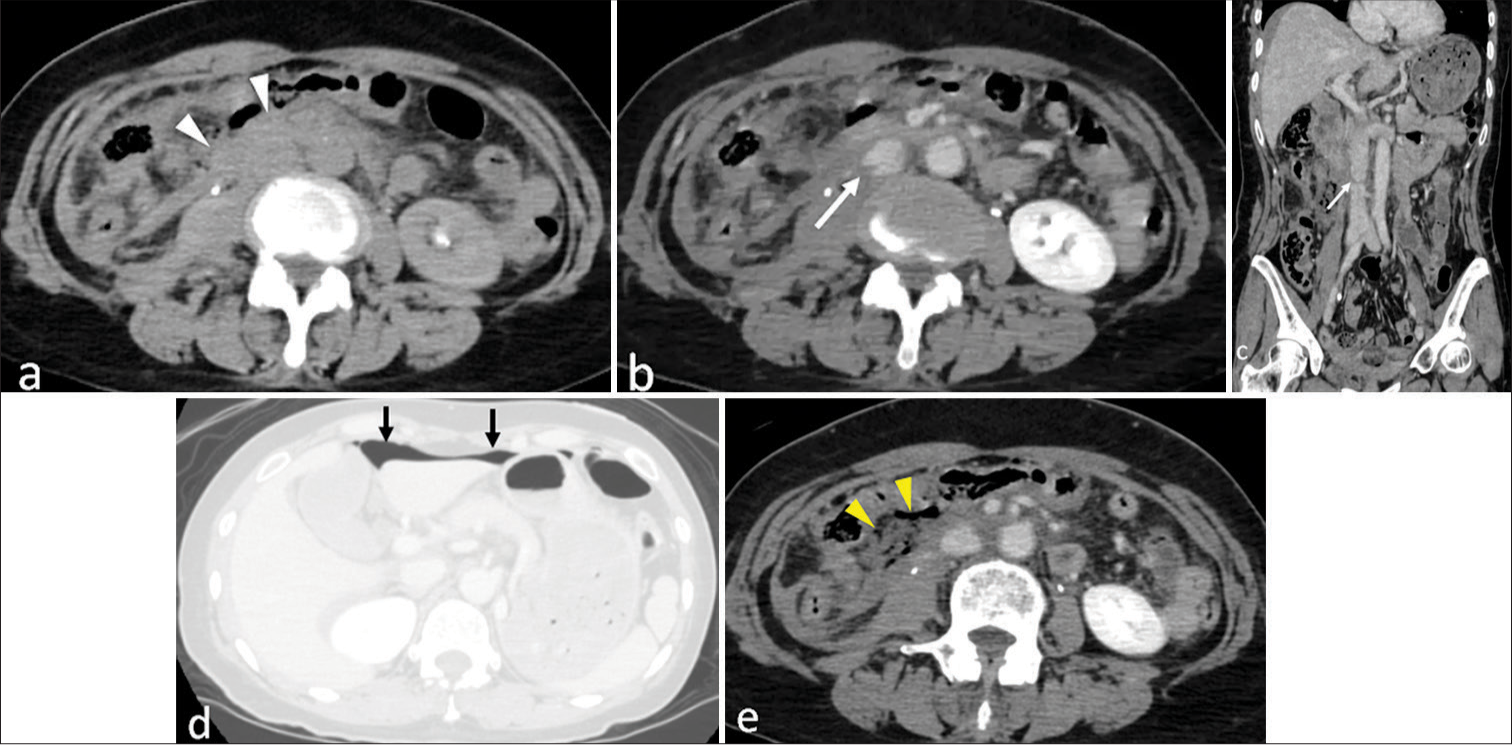
CASE REPORTA 57-year-old woman with no significant medical history was transported to our hospital after being involved in a head-on collision while seated in the front passenger seat of a car traveling at 50 km/h with a seatbelt fastened. Physical examination revealed subcutaneous hematomas in the right hypochondrium and left lower abdomen. The Glasgow coma scale (GCS) score was 15, and the patient exhibited quadriparesis. Her blood pressure was 106/61 mmHg, and her pulse rate was 73 bpm. Laboratory findings included a hemoglobin level of 10.4 g/dL, indicating mild anemia, and a platelet count of 139,000/μL, which was within the lower normal range. Coagulation studies revealed a markedly elevated D-dimer level of 40.25 μg/mL, suggestive of significant fibrinolytic activation, and a low fibrinogen level of 96.30 mg/dL, indicating consumptive coagulopathy. The activated partial thromboplastin time (22.9 s), prothrombin time (13.9 s), and prothrombin time-international normalized ratio (1.10) were within normal limits. A head CT scan performed on the day of injury showed no traumatic changes. Contrast-enhanced chest and abdominal CT revealed a retroperitoneal hematoma around the IVC and an irregular contour of the infrarenal IVC, suggesting a blunt traumatic IVC injury [Figure 1]. Free air in the abdominal cavity and a small amount of hemoperitoneum in the pelvis suggested bowel perforation [Figure 1]. Magnetic resonance imaging revealed C5–C6 subluxation and spinal cord injury at the same level, with associated bilateral facet subluxations and no vertebral body fracture. This combination of injuries may raise suspicion for a seatbelt injury pattern, which is typically caused by rapid deceleration and flexion-compression forces.
Export to PPT
Surgery for bowel perforation was performed on the day of injury, including partial resection of the small bowel and transverse colon. The small bowel was completely transected approximately 50 cm from the Treitz ligament and was resected. The transverse colon had ischemic changes at the mesenteric injury site and was also partially resected. A retroperitoneal hematoma extending from the duodenum to the right renal vein was observed, which was suspected to be due to a blunt traumatic IVC injury. There was no rupture of the retroperitoneal hematoma into the peritoneal cavity. Although endovascular stenting is available and has been utilized in other institutions for similar cases, conservative management was chosen in this case due to the patient’s hemodynamic stability, the absence of active contrast extravasation, and the self-limiting nature of the retroperitoneal hematoma. There were no facility limitations. Follow-up contrast-enhanced CT on day 5 post-injury showed a reduction in the retroperitoneal hematoma, improvement in the irregular contour of the infrarenal IVC, and no extravasation of contrast medium [Figure 2]. Spinal fixation from C3 to C7 was performed on day 2 post-injury. The patient’s quadriparesis improved to the extent that she was able to transfer to a wheelchair. She was transferred to a rehabilitation facility on day 26 post-injury. A summary of the clinical course is presented in Table 1.

Export to PPT
Table 1: Clinical time course.
Day Examination (imaging only) Treatment/Outcome 0Head CT
Contrast-enhanced CT
IVC injury
MRI
• Partial resection of small bowel and transverse colon 2 N/A • Cervical spinal fixation (C3–C7) 5 26 N/A • Transferred to rehabilitation facility DISCUSSIONIVC injuries have been reported in 0.5% to 5% of cases of penetrating trauma;[9] however, the incidence of blunt trauma-related IVC injuries remains unclear and is considered extremely rare.[10] Overall mortality for IVC injuries is high, with 30–50% of patients dying before reaching the hospital and 20–57% of hospitalized patients not surviving their injuries.[3,11] Blunt traumatic IVC injuries are frequently associated with multiple organ injuries, with the liver being the most commonly affected, followed by gastrointestinal and diaphragmatic injuries.[3,12] In the present case, the blunt traumatic IVC injury resulted from a traffic accident and was accompanied by gastrointestinal and spinal cord injuries. The gastrointestinal injury required surgical intervention, while the IVC injury was successfully managed with non-operative conservative treatment, allowing for the patient’s survival and subsequent rehabilitation.
CT findings of IVC injury include extravasation of contrast media, retroperitoneal hematoma, and IVC contour abnormalities.[10] The extravasation of contrast media suggests active bleeding, while a retroperitoneal hematoma is the most common finding, observed in 75% of cases. IVC contour abnormalities, such as irregular contour or deformation of the vessel wall, are critical signs indicative of IVC injury. These abnormalities are observed in 50% of blunt trauma cases and 17% of penetrating trauma cases.[10] In this case, the presence of a retroperitoneal hematoma and IVC contour abnormalities was observed. Despite the absence of extravasation of contrast media, recognizing these findings was crucial for diagnosing IVC injury.
The treatment strategy for IVC injuries depends on the location and extent of the injury as well as the patient’s hemodynamic status. Non-operative conservative management is considered when the patient is hemodynamically stable and the bleeding is contained within the retroperitoneum, with spontaneous hemostasis potentially occurring due to the hepatic capsule or diaphragm.[10] We reviewed previously reported cases of blunt IVC injuries managed either conservatively or surgically to better contextualize the present case. As shown in Table 2,[13-15] the number of conservatively managed cases is limited, and all reported a 0% mortality rate. In contrast, Table 3 summarizes outcomes of surgically managed cases, in which mortality rates ranged from 0% to over 78.6%, depending on the study.[16-25] Although the available data on conservative management remain limited, these findings suggest that it may be a reasonable option in carefully selected, hemodynamically stable patients with infrarenal IVC injuries. The IVC is a low-pressure retroperitoneal structure, and early bleeding may be tamponaded within the retroperitoneum.[26] Direct repair with sutures is typically performed when the patient is hemodynamically unstable and the injury is limited in size. However, injuries to the retrohepatic IVC are particularly challenging, with high mortality rates. In cases involving complex injuries to the retrohepatic IVC, shunt or bypass procedures using cardiopulmonary bypass or venous shunts may be required.[27,28] Endovascular treatment, including stent graft repair[6] and balloon occlusion for hemorrhage control,[29] is an option in hemodynamically stable patients or when surgery is undesirable. Recent reports have also described the use of extracorporeal membrane oxygenation as a novel approach.[30] The decision-making process should consider the location of the IVC injury (retrohepatic, suprarenal, or infrarenal) and the presence of associated injuries (e.g., liver injury), which can be assessed using CT imaging, as well as the patient’s hemodynamic stability. In this case, the IVC injury was located in the infrarenal region, with no extravasation of contrast media, and the patient remained hemodynamically stable. Although endovascular stenting was considered, conservative management was chosen. During the laparotomy for bowel perforation, there was no rupture of the retroperitoneal hematoma into the peritoneal cavity.
Table 2: Conservative management of blunt IVC injuries in previous reports.
Study Sample size Mortality rate (%) Injury location Duncan et al., 2005[13] 1 0 Infrarenal Netto et al., 2006[14] 1 0 No mention found Turpin et al., 1977[15] 1 0 No mention foundTable 3: Surgical management of blunt IVC injuries in previous reports.
Study Sample size Mortality rate (%) Management type Byerly et al., 2019[26] 443 Ligation: 23, Repair: 16 Ligation vs. Repair Coimbra et al., 1994[19] 49 39 Various surgical approaches Klein et al., 1991[27] 38 21 Open surgical repair Kuehne et al., 1999[2] 100 52 Repair, Ligation Leppäniemi et al., 1994[28] 16 37.50 Open repair, Ligation Liu et al., 2005[29] 19 42 Open surgical repair Matsumoto et al., 2018[30] 1,316 Ligation: 41.3, Repair: 39.0 Ligation vs. Repair Ombrellaro et al., 1997[31] 27 48 Open repair, Ligation Park and Kim, 2023[13] 14 78.60 Open repair, Ligation Rosengart et al., 1999[32] 37 51 Lateral repair, Ligation, Gortex graft Stonko et al., 2021[33] 140 42 Open repair, Ligation Sullivan et al., 2010[34] 25 59 IVC ligation Wu et al., 2000[35] 6 0 Open surgical repairMortality risk factors for blunt traumatic IVC injury include a low GCS score and the need for massive red blood cell transfusion within 24 h.[31] Among injury locations, retrohepatic IVC injuries are the most fatal, with mortality rates reaching 70–100%.[32] Suprarenal IVC injuries also have high mortality rates, ranging from 67 to 100%.[32] In contrast, infrarenal IVC injuries have a relatively lower mortality rate of 20–39%. In this case, the injury was located in the infrarenal IVC, with a GCS score of 15 and no requirement for massive transfusion, suggesting a lower risk profile. Recognizing CT findings of IVC injury and making appropriate treatment decisions are crucial. Reports of successful non-operative management of blunt traumatic IVC injuries remain limited, highlighting the need for further case accumulation.
The combination of injuries observed in the present case, including bowel perforation and IVC injury, suggests the possibility of a seatbelt-associated mechanism. Bowel perforation is a well-documented finding in seatbelt injuries, typically resulting from the transmission of compressive forces between the seatbelt and the abdominal organs during abrupt deceleration.[33] Although seatbelt-associated IVC injury is extremely rare,[34] it is anatomically plausible and has been reported in isolated cases. In contrast, the cervical spine injury is more likely attributable to the dynamics of the collision itself, such as hyperflexion or axial loading, rather than direct force from the seatbelt.[35] Taken together, these findings indicate a complex injury pattern likely caused by a combination of deceleration, compression, and flexion forces, partially consistent with a seatbelt injury mechanism.
CONCLUSIONBlunt traumatic IVC injury is rare. Even in the absence of extravasation of contrast media, recognizing retroperitoneal hematoma and IVC contour abnormalities is critical for diagnosis. A comprehensive assessment of the patient’s overall condition and CT findings (IVC injury location and associated injuries) is essential in determining the appropriate treatment approach, as demonstrated in this successfully managed case.
Comments (0)