A 19-year-old patient was admitted due to loss of consciousness. The chronological progression of symptoms is outlined in Figure 1. On examination, the Glasgow Coma Scale was 10 points (eye opening 4, motor response 5, verbal response 1). The patient’s blood pressure was 120/89 mmHg, and the heart rate was 112 bpm. She denied any respiratory, gastrointestinal, or urogenital infections. There was no history of trauma, and no bruising or purpura were observed on the skin. Neurological examination showed pupils measuring 3 mm with intact light reflexes; neck stiffness and Babinski signs were negative. A bedside glucose test revealed 131 mg/dL. Head computed tomography (CT) revealed no intracranial lesions. Electroencephalography showed bifocal slow-wave activity. Meningoencephalitis was the primary diagnosis, with microvascular stroke considered as a differential diagnosis.
Table 1Laboratory results of the patient on admission day
Total blood count
Cerebrospinal fluid (CSF) analysis
Red blood cell
4.44 (T/L)
CSF glucose
65 (mg/dL)
Hemoglobin
132 (g/L)
CSF lactate
16.8 (mg/dL)
White blood cell
12.09 (G/L)
CSF protein
27.2 (mg/dL)
Neutrophil count
10.41 (G/L)
CSF-to-blood glucose ratio
0.677
Lymphocyte count
0.84 (G/L)
ADA
0.3 (U/L)
Monocyte count
0.67 (G/L)
Eosinophil count
0.03 (G/L)
Basophil count
0.02 (G/L)
Platelet count
301 (G/L)
Immunological test
Anti ds-DNA
4.58 (IU/ml)
Anti-Sm
0.29 (U/ml)
Cardiolipin IgG
<2.0 (U/ml)
Cardiolipin IgM
2.5 (U/ml)
fT3
2.06 (pg/ml)
fT4
14 (pg/ml)
TSH
0.49 (mIU/L)
ANA
Negative
Blood IFT for autoimmune encephalitis
CSF IFT for autoimmune encephalitis
GABA-RB1/B2
Negative
GABA-RB1/B2
Negative
LGI1
Negative
LGI1
Negative
CASPR2
Negative
CASPR2
Negative
DPPX
Negative
DPPX
Negative
AMPA-R1/R2
Negative
AMPA-R1/R2
Negative
NMDAR
Positive
NMDAR
Positive
Diagnostic WorkupA complete blood count was performed to screen for infection and adverse treatment events. Cerebrospinal fluid (CSF) aspiration yielded no bacterial or fungal growth; blood culture findings were consistent with polymerase chain reaction assays for M. tuberculosis or Herpes simplex virus. No evidence of microvascular stroke was detected on magnetic resonance imaging (MRI). Thus, both infectious meningoencephalitis and stroke were deemed unlikely. Detailed laboratory findings are presented in Table 1.
The diagnostic focus then shifted toward autoimmune etiology. Serum autoantibody tests, including anti-ds-DNA, anti-SM, and anti-phospholipid, were negative. However, anti-NMDAR IgG was positive in both serum (screening at 1:10) and CSF (screening at 1:1), confirming NMDAR encephalitis. Concurrently, pelvic CT revealed a 29 × 21 mm fluid-density mass in the left ovary. Surgery was deemed too high risk due to the patient’s critical status, and thus histopathologic features of the tumor could not be determined.
According to institutional policy, ethical approval for this single anonymized case report was not required; however, written informed consent was obtained from the patient’s legal guardian for both treatment and publication, including use of anonymized data.
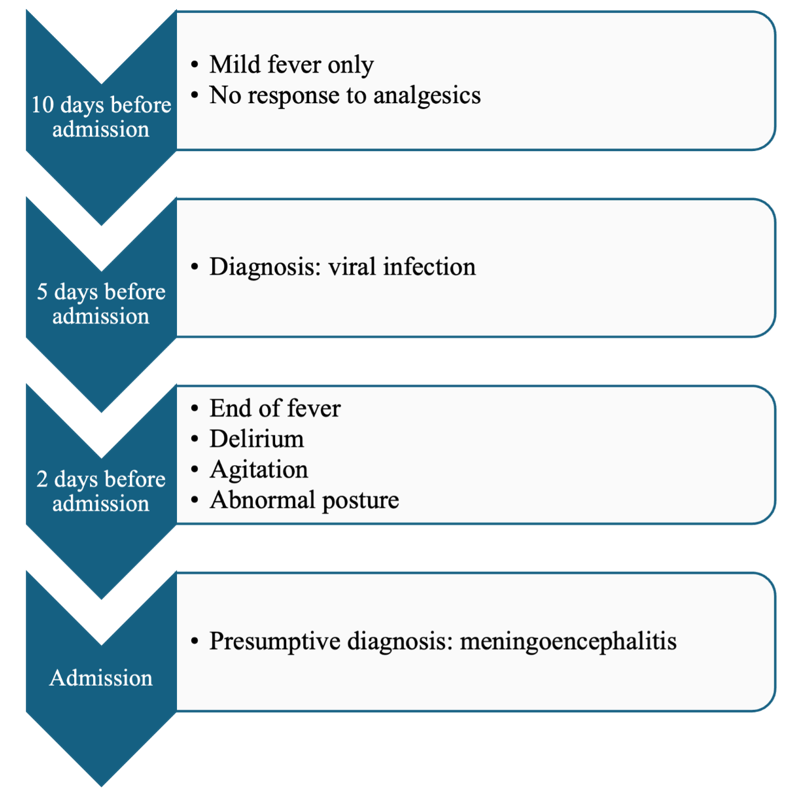 Figure 1
Figure 1 Symtomp presentation in chronological order.
Treatment and OutcomeUpon admission, the patient was unable to communicate effectively due to agitation and delirium. Treatment comprised intravenous immunoglobulin, midazolam, and high-dose methylprednisolone, although symptom progression was only slowly alleviated. Plasmapheresis was then initiated; during the procedure, purpura appeared on both limbs but resolved rapidly. After seven plasmapheresis sessions, the patient recovered consciousness and displayed neurological improvement, including the ability to breathe spontaneously and tolerate oral nutrition. She experienced a few intermittent catatonic episodes. Following 23 days of treatment, she was discharged with marked clinical improvement (Table 2). In March 2025, a follow-up examination revealed a Beck’s Depression Inventory score of 1, suggesting no depression, and a Mini-Mental State Examination score of 28, indicating no cognitive impairment.
Table 2Summary of treatment regimen
IV Immunoglobulin
0.4 g/kg/day
5 days
No significant improvement
Corticosteroid
Methyl prednisolone 1g/day
5 days
High-dose pulse therapy
Plasmapheresis
Single volume exchange
Every other day,
7 sessions total
Significant clinical improvement
Symptomatic (sedation)
Midazolam infusion
PRN
Used during agitation
DiscussionSince first reported in 2008, anti-NMDAR encephalitis has become one of the most common forms of autoimmune encephalitis, particularly in young females. It involves autoantibodies against the GluN1 subunit of NMDA receptors, manifesting a broad spectrum of neuropsychiatric symptoms. Multiple investigations have documented its association with ovarian teratomas, which may harbor neural tissue and elicit an immune response. Comprehensive tumor screening is therefore standard in the diagnostic process1, 2, 3.
This patient presented similarly to previously documented cases, with a viral-like prodrome, rapid onset of neuropsychiatric manifestations, anti-NMDAR antibodies in both serum and CSF, and no evident infectious or structural etiology. Pelvic CT identified a cystic lesion in the left ovary, consistent with a tumor, although the patient’s unstable status precluded surgical resection and histopathological confirmation. Consequently, the direct role of the lesion in antibody production cannot be definitively established. Future cases should undergo histological evaluation when clinically feasible to refine diagnostic accuracy.
Despite the unresolved tumor status, the patient responded well to high-dose corticosteroids and plasmapheresis. Because initial intravenous immunoglobulin therapy did not prompt significant improvement, plasma exchange was introduced, consistent with current first-line therapeutic recommendations1, 5. Rituximab was not employed due to limited availability and its usual role as a second-line agent. Other reports in resource-limited settings describe favorable outcomes using a steroid–plasmapheresis combination when surgical or biologic options are not viable6, 7.
Symptom resolution and seroconversion (loss of anti-NMDAR IgG) despite retaining the ovarian lesion raise important questions regarding underlying antibody production mechanisms. Despite a plausible tumor relationship, potential alternatives include transient tumor-mediated autoimmunity, intrathecal synthesis of antibodies independent of peripheral triggers4, or post-infectious immune processes8, 9, 10. Anti-NMDAR encephalitis has additionally been observed in males, children, and adults without detectable tumors11, 12, 13, indicating that non-paraneoplastic mechanisms may also be involved.
At six-month follow-up, the patient demonstrated complete neurological and psychiatric recovery with negative serum anti-NMDAR IgG. However, imaging showed persistence of the ovarian lesion. Given the higher relapse risk in patients whose tumors remain in situ5, a structured surveillance plan was initiated, involving quarterly neuropsychiatric assessments and antibody monitoring for one year, then biannual evaluations. Surgical management will be reconsidered if there is any sign of progressive lesion growth or clinical relapse. Mental health screening remains a priority, given the potential for subclinical recurrence arising from residual low-titer antibodies14, 15, 16, 17, 18, 19, 20.
This case report demonstrates a rare example of successful non-surgical management of anti-NMDAR encephalitis, with comprehensive diagnostic, therapeutic, and follow-up protocols. Strengths include reliable exclusion of alternate diagnoses, a clear treatment rationale, and applicability to resource-limited settings.
Nonetheless, several limitations must be acknowledged. Without histopathological data on the ovarian lesion, definitive conclusions regarding the source of antibody production cannot be made. As a single case, its findings cannot be universally applied. Additionally, while the patient remained relapse-free at six months, longer-term outcomes remain unknown, and the absence of serial CSF antibody titers impedes more detailed immunological insight.
Comments (0)