Thyroid nodules are a commonly observed condition in clinical practice with a complex etiology and can be classified as benign or malignant.[1] Related research results show that the incidence of malignant nodules in patients with thyroid nodules is approximately 5.6–79.8%.[2] Compared with patients with benign nodules, patients with malignant thyroid nodules have more serious conditions, and their physical and mental health and quality of life are affected,[3-6] so timely identification of the pathological natures of thyroid nodules is vital.
The puncture technique was first used in the pathological examination of tumors in 1930 and was adopted in the cutting biopsy of thyroid diseases in the 1950s and 1960s. However, traditional coarse needle biopsy can lead to complications or metastasis of tumor cells along the needle tract, limiting its clinical application.[7-9] Fine-needle aspiration biopsy (FNAB) is a newer technique that offers minimal injury, reduced pain, and ease of operation. FNAB effectively mitigates the complications and metastasis risks associated with coarse needle biopsy, thus reducing the need for unnecessary surgeries. Consequently, it has gradually become the biopsy technique recommended by clinical guidelines.[10-12] Hence, higher requirements are placed on the puncture path and site accuracy because of the limited tissue dose obtained by fine-needle aspiration.
With the continuous improvement of modern medical technology and ultrasound equipment, ultrasound technology has also been used in thyroid nodule examination, which shows an increasing trend in the detection rate of nodules.[13-15] Ultrasound-guided fine-needle aspiration cytology (USFNAC) is a minimally invasive technique that effectively diagnoses the nature of thyroid nodules. Unfortunately, clinical reports on the diagnostic value of US-FNAC in determining the nature of thyroid nodules are scarce, and the relationship between the diagnostic efficacy of US-FNAC and nodular diameter has not been established. In this study, the result of post-operative pathological examination was the gold standard for analyzing the value of US-FNAC in diagnosing benign and malignant thyroid nodules and exploring its application effect in nodules of different sizes. This study aims to provide an effective reference for improving the accuracy of clinical diagnosis of nodular natures, determining treatment options, and evaluating prognosis.
MATERIAL AND METHODS Inclusion and exclusion criteria Inclusion criteriaAdult patients with thyroid nodules diagnosed by ultrasound, those undergoing resection surgery of thyroid nodules for the first time, those with basic listening, speaking, reading, and writing abilities, and those with complete clinical data were included.
Exclusion criteriaPatients with infection or skin injury at the puncture site after US-FNAC, puncture failure, cognition or communication disorders, incomplete clinical data, treatments such as sclerosing agent injection, drugs, radiofrequency ablation before enrollment, the history of radiotherapy and tumor surgery, distant metastasis of malignant tumors, severe diseases in heart, liver and kidney or other tumor types, and those in lactation period or gestation period were excluded.
Study methodsThis retrospective study was approved by the medical ethics committee of Zibo Central Hospital (approval no.: 2024052). Considering the anonymity of data, patients informed consent was waived. The study was conducted in accordance with the Declaration of Helsinki.
A total of 116 patients underwent thyroidectomy in Zibo Central Hospital from January 2022 to March 2023, whose eligibility was evaluated according to the inclusion and exclusion criteria to determine the study subjects. Clinical data and information related to ultrasound imaging, diagnosis and treatment of cytopathology, and post-operative pathological examination were collected for each subject. The ultrasound features of patients with benign and malignant nodules were compared. Taking the result of post-operative histopathologic examination as the gold standard, the area under the curve (AUC) value was calculated via receiver operator characteristic (ROC) curve to determine the diagnostic value of US-FNAC for the pathological natures of thyroid nodules.
Finally, the patients were divided into groups Q1, Q2, Q3, and Q4 according to the median and quartile of nodular diameters to further evaluate US-FNAC’s diagnostic efficacy for the pathological natures of thyroid nodules with different diameters.
Examination and evaluation methods Surgical pathological examination and evaluationDuring the resection of thyroid nodules, all patients underwent resection of lesion nodules under general anesthesia, and a rapid pathological examination of diseased thyroid tissues was carried out. The collected specimens were transferred to the pathology department for assessment by two experienced pathologists at the level of attending physician or above. Consultation was necessary to obtain a unified diagnostic result if different opinions existed.
Typical cancer cells in the specimens were assessed as malignant, and non-typical cancer cells were assessed as benign.
Ultrasound examination and evaluationThe color ultrasound diagnosis equipment (model: Philips EPQ5) with L12–5 probe was selected for ultrasound examination, and the probe frequency was 5–12 MHz. The patient was guided to adopt a supine position, and the pillow was placed behind the patient’s neck to tilt the head backward. After fully exposing the neck skin, ultrasound detected the bilateral thyroid lobes and isthmus and observed nodular location, size, number, morphological characteristics, blood flow, internal echo, and calcification situations.
According to the American Thyroid Association (ATA) guidelines, the ultrasound examination results could be divided into five types.[16]
BenignSimple cystic nodules (no solid component).
Super-low suspected malignancySpongiform or partially cystic nodules without any of the ultrasound features described in low, moderate, or high suspected pattern.
Low suspected malignancySolid nodules with equal or high echo or partially cystic nodules with eccentric solidity. Moderate suspected malignancy
Solid nodules with low echo and smooth margins.
High suspected malignancySolid nodules (components) with a low echo of a partially cystic nodule with one or more of the characteristics including irregular edges (infiltrative, microlobulated), microcalcification, longer than wide shape, edge calcification combined with small prominent soft tissue component, and the evidence of extrathyroid extension.
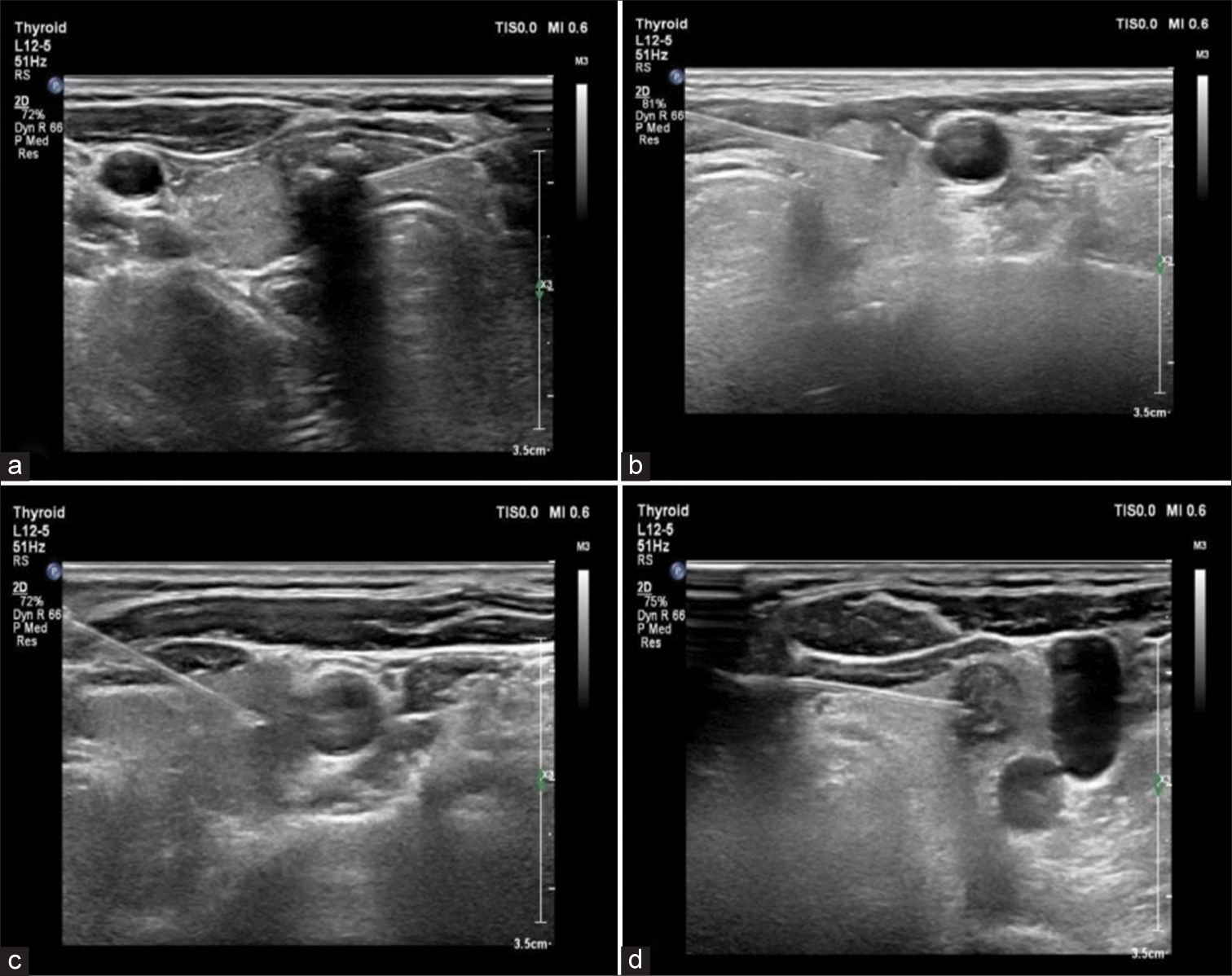
US-FNAC examination and evaluationAccording to the results of clinical and ultrasound examinations, the most suspected thyroid nodule was examined through US-FNAC. After disinfection and towel treatment, 2% lidocaine (NMPA approval no.: H37022114; specification: 5 mL: 0.1 g, manufacturer: Shandong Hualu Pharmaceutical Co., Ltd.; origin: Liaocheng, China) at a dose of 50–300 mg was used for local infiltration anesthesia. A 22 G fine needle was selected to puncture the corresponding suspected nodules under ultrasound guidance [Figure 1]. The multi-directional puncture should reach the nodular internals to obtain contents as much as possible. Negative pressure suction was reasonably adopted if the tissue was difficult to extract. If the aspirate contained more blood, the remaining blood was aspirated completely from various directions using a syringe after slightly shaking the glass slide, and then, the suction operations were performed three times, subsequently obtaining specimens. The syringe was withdrawn, the needlepoint was pressed with gauze, and the specimens were placed in the slide, and the slide method was used for examination. Two experienced pathologists (attending physician or above) evaluated the results. When there were different opinions, consultation was needed, and the final diagnosis results were obtained after the unification of opinions.
Export to PPT
According to US-FNAC results, patients could be divided into the following six types.[17]
Patients with non-diagnostic or unsatisfactory specimen results were classified as type I
Patients with benign lesions were classified as type II
Patients showing atypical cellular lesions with unclear diagnostic significance were classified as type III
Patients with suspected or existing follicular tumors belonged to type IV
Patients with suspected malignant tumors were classified as type V
Patients with definitely diagnosed malignant tumors were classified as type VI.
Statistical analysisThe pre-operative US-FNAC and post-operative paraffin pathology results of all patients with thyroid nodules were entered into the SPSS database (version: 26.0, developer: IBM Corporation; Armonk, State of New York, USA). The categorical variables were expressed as (n [%]) and tested by Fisher’s exact probability or the correction formula of the chi-square test, and continuous variables were tested by the Shapiro–Wilk test and the data meeting non-normal distribution were expressed as M (P25, P75). ROC curves were used to evaluate the diagnostic efficacy of US-FNAC. When AUC > 0.5, the AUC closer to 1 indicates a better diagnostic effect (i.e., AUC = 0.5–0.7 indicates low accuracy, AUC=0.7–0.9 indicates a certain accuracy, and AUC > 0.9 indicates high accuracy). Microsoft Office Word 2006 (Microsoft Corporation; Redmond, WA, USA) and SPSS software were used to create figures.
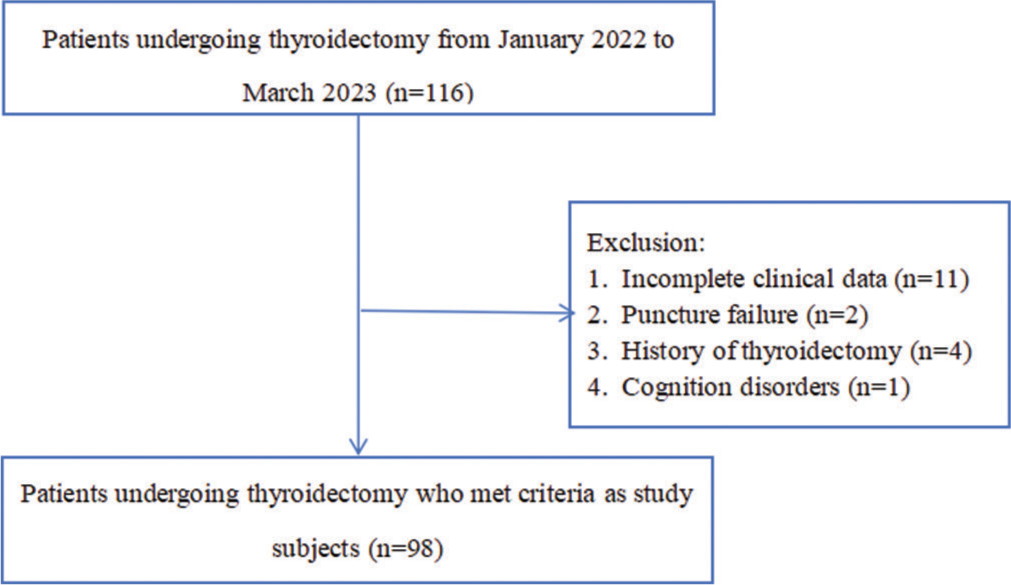
RESULTS Baseline dataThis study selected a cohort of 116 patients, of which 98 met the inclusion criteria [Figure 2]. Of these, 53 were female (54.08%) and 45 were male (45.92%), with an average age of 53.46 ± 6.62 years (ranging from 32–76 years).
Export to PPT
Results of surgical pathological examinationIn this study, 98 nodules were punctured, with a diameter of 0.8–5.2 cm and a median and quartile of (1.98 ± 0.70) cm, including 10 (10.20%) benign nodules and 88 (89.80%) malignant nodules, as shown in Table 1.
Table 1: Results of surgical pathological examination.
Surgical results Pathological types NumberAccording to ATA guidelines, 98 thyroid nodules were classified, including 14 (14.29%) benign nodules and 84 (85.71%) suspected malignant nodules. The specific ultrasound classification results are shown in Table 2. The composition, echo, calcification, edge, and shape of benign thyroid nodules were significantly different from those of malignant thyroid nodules (P < 0.05), and the specific ultrasonic features are shown in Table 3.
Table 2: Ultrasound classification of thyroid nodules.
Ultrasound classification Number (n[%]) Benign 14 (14.29) Super-low suspected malignancy 16 (16.33) Low suspected malignancy 28 (28.57) Moderate suspected malignancy 11 (11.22) High suspected malignancy 29 (29.59) US-FNAC RESULTSTable 3: Ultrasonic features of thyroid nodules (n [%]).
Ultrasonic features Number (n=98) Surgical pathological results χ2/Fisher P-value Benign (n=10) Malignant (n=88) Composition Solid-cystic 20 (20.41) 5 (50.00) 15 (17.05) 4.146 0.042 Solid 78 (79.59) 5 (50.00) 73 (82.95) Echo Low/super-low echo 70 (71.43) 4 (40.00) 66 (75.00) 4.830 0.028 Equal/high echo 28 (28.57) 6 (60.00) 22 (25.00) Calcification Micro calcification 44 (44.90) 1 (10.00) 43 (48.86) Fisher 0.034 Coarse calcification 15 (15.31) 3 (30.00) 12 (13.64) No calcification 39 (39.80) 6 (60.00) 33 (37.50) Edge Irregular edge 76 (77.55) 5 (50.00) 71 (80.68) 4.132 0.042 Smooth/regular edge 22 (22.45) 5 (50.00) 17 (19.32) Shape Aspect ratio<1* 25 (25.51) 8 (80.00) 17 (19.32) 14.354 <0.001 Aspect ratio>1# 73 (74.49) 2 (20.00) 71 (80.68)The US-FNAC results of 98 thyroid nodules showed 9 (9.18%) benign nodules, 84 (85.72%) malignant nodules, and 5 (5.10%) uncertain pathological natures, as shown in Table 4 and Figure 3.
Table 4: Pathological results of US-FNAC and surgery (n [%]).
Classifications Pathological natures Total Type I Uncertain 2 (2.04) Type II Benign 9 (9.18) Type III Uncertain 3 (3.06) Type IV Malignant 29 (29.59) Type V Malignant 39 (39.80) Type VI Malignant 16 (16.33)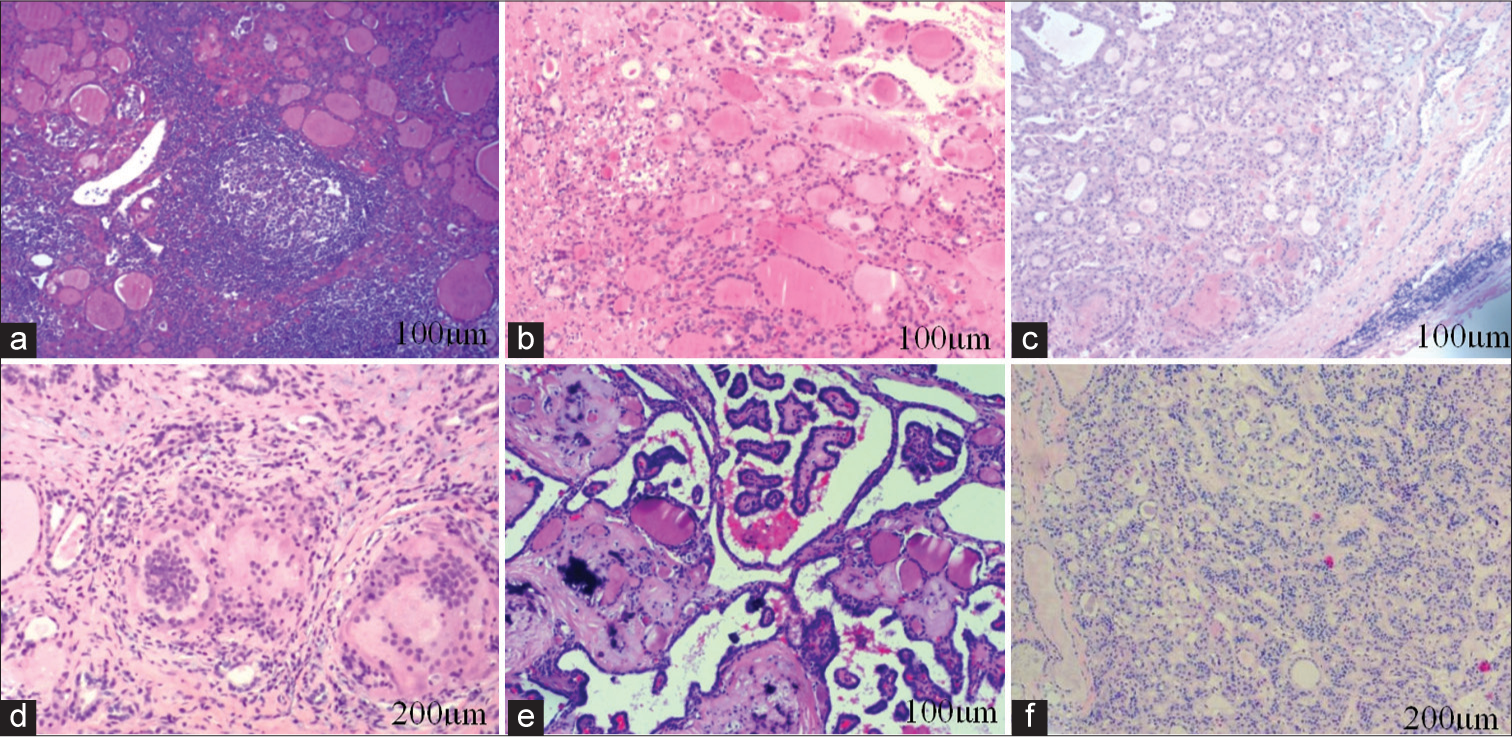
Export to PPT
Diagnostic efficacy of US-FNAC for the pathological natures of thyroid nodulesBecause the benign and malignant natures of nodules in type I and type III could not be determined, 93 cases were included after excluding nodules in type I and III. The result of the post-operative pathological examination was used as the gold standard for ROC analysis, showing that the AUC, sensitivity, specificity, and 95% confidence interval of US-FNAC were 0.894, 98.80%, 80.00%, and 0.745–1.000, respectively, as shown in Table 5 and Figure 4.
Table 5: Diagnostic efficacy of US-FNAC for the pathological natures of thyroid nodules.
Benign Malignant AUC Sensitivity (%) Specificity (%) 95% CI US-FNAC (n=93) Benign 8 1 0.894 98.80 80.00 0.745~1.000 Malignant 2 82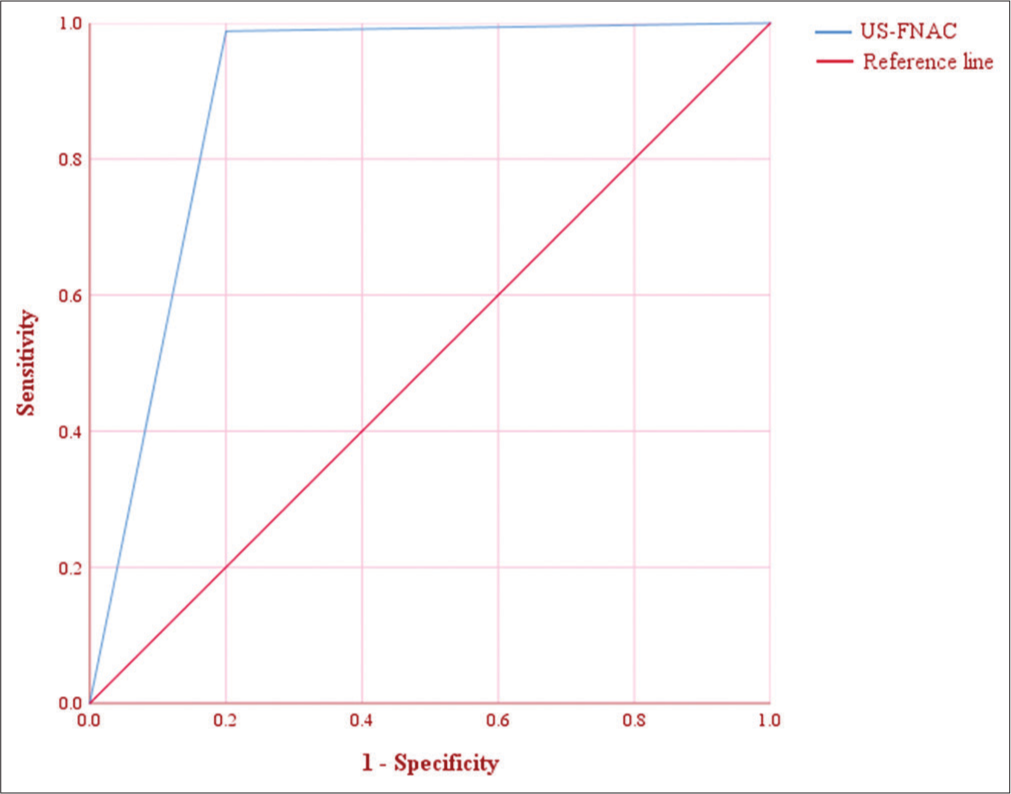
Export to PPT
Diagnostic efficacy of US-FNAC for pathological natures of thyroid nodules with different diametersAccording to the median and quartile of nodular diameters, i.e., 1.90 (1.60, 2.30) cm, 93 patients were divided into groups Q1 (≤1.6 cm), Q2 (1.7–1.9 cm), Q3 (2.0–2.3 cm), and Q4 (>2.3 cm). The results of ROC analysis showed that the AUCs of US-FNAC in the above groups were 0.978, 1.000, 0.977,0.971. The AUCs of Q1 group, Q2 group, Q3 group and Q4 group were all > 0.9, and US-FNAC had high diagnostic efficiency for the pathological properties of thyroid nodules with different diameters, as shown in Table 6 and Figure 5.
Table 6: Diagnostic efficacy of US-FNAC for pathological natures of thyroid nodules with different diameters.
Groups Surgical pathological examination results AUC Sensitivity (%) Specificity (%) 95% CI Benign Malignant Group Q1 (n=24) Benign 1 1 0.978 95.70 100.00 0.914-1.000 Malignant 0 22 Group Q2 (n=26) Benign 3 0 1.000 100.00 100.00 0.000 –1.000 Malignant 0 23 Group Q3 (n=24) Benign 2 0 0.977 100.00 66.70 0.818-1.000 Malignant 1 21 Group Q4 (n=19) Benign 2 0 0.971 100.00 66.7 0.774-1.000 Malignant 1 16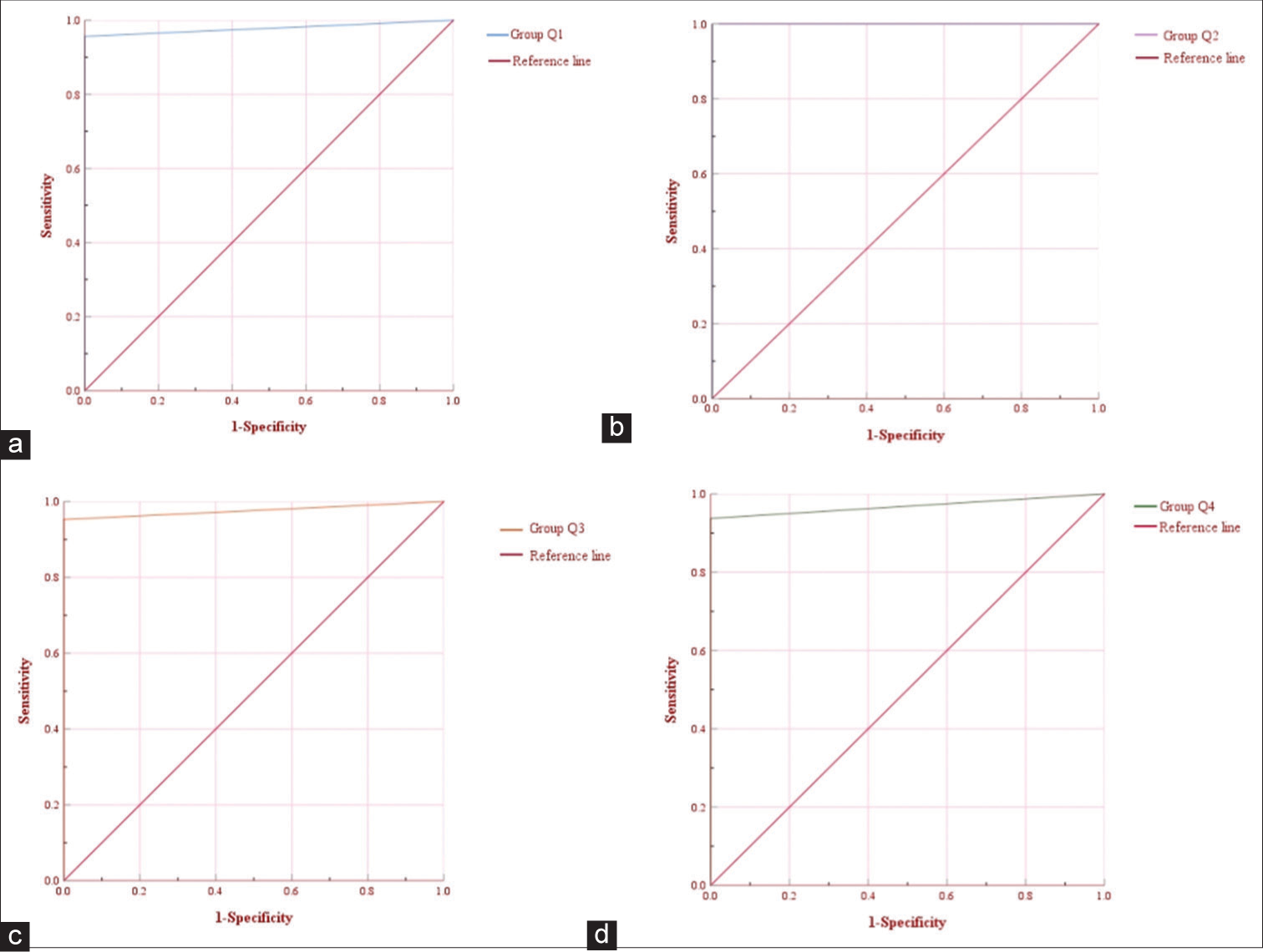
Export to PPT
DISCUSSIONFine-needle aspiration cytology and ultrasonic examination are key tools for pre-operative evaluation of patients with thyroid lesions.[18-20] Ultrasound examination provides a reference for nodular selection in US-FNAC. Ultrasound guidance assists physicians in seeking a more accurate puncture path and the best puncture position, thus effectively avoiding blood vessels and nerves and improving the success rate of puncture while ensuring safety. In comparison with palpation-guided fine-needle aspiration cytology, USFNAC has higher accuracy.[21] A foreign study indicated that ultrasound features such as low echo, fine calcification, irregular edge, and nodular aspect ratio >1 were potential indicators of malignant thyroid nodules.[22] This is consistent with the result of the analysis of this study, which fully confirms the application value of ultrasonic examination in fine-needle aspiration cytology of thyroid nodules.
The US-FNAC results in this study showed 9 (9.18%) benign nodules, 84 (85.72%) malignant nodules, and 5 (5.10%) nodules with uncertain pathological natures 2 (2.04%) specimens had unsatisfactory diagnoses, and 3 (3.06%) specimens were atypical cellular lesions with unclear diagnostic significance). According to surgical pathology results, two benign nodules and one malignant nodule were not correctly diagnosed in this study, including that two nodules were diagnosed as Hashimoto’s thyroiditis by pre-operative US-FNAC but were diagnosed as papillary carcinoma by surgery. Hou et al.[23] have also obtained similar results, finding that Hashimoto’s thyroiditis, a risk factor for the increase of false-negative rate, would reduce the diagnostic accuracy of US-FNAC. There may be two main reasons for this phenomenon, uniform lesions can result in omission during the puncture process, and second, insufficient experience among physicians can lead to incorrect cytopathologic diagnoses. In addition, one nodule was diagnosed with a malignant tumor by pre-operative USFNAC but was diagnosed as Hashimoto’s thyroiditis by surgical pathology, speculating that it may be related to the limitations of US-FNAC. US-FNAC is based on ultrasonic features, but some benign nodules are easily misdiagnosed as malignant tumors because of irregular edges and uneven echoes.
It has been reported that the accuracy of US-FNAC may also be affected by the size of thyroid nodules.[24,25] In response to this problem, this study divided the patients into four groups according to the median and quartile. Statistical analysis found the AUCs of groups Q1, Q2, Q3, and Q4>0.9, and USFNAC had high diagnostic efficiency for the pathological properties of thyroid nodules with different diameters. We speculate that this may be related to the small number of cases in our study. The needle may slide out of the nodule during sampling or enter the normal tissue. In addition, Zhao et al.[26] point out that nodular size has a certain effect on the positive rate of fine needle aspiration, mainly due to the lower diagnostic efficiency of conventional ultrasound on suspected malignant features in small nodules. Therefore, it is necessary to actively perform long-term follow-up for patients with thyroid nodules in types I and III through US-FNAC and patients with small nodular diameters and perform repeat punctures if necessary.
However, US-FNAC diagnosis is also susceptible to factors such as clinical physicians’ diagnostic experience and proficiency.[27-29] In this study, two patients were excluded due to inexperienced physicians who caused puncture failure, with an incidence of 1.90% (2/105) when screening patients, and this situation needs attention, although the incidence is not high. It is advocated that experienced physicians should perform US-FNAC, and patients should experience comprehensive evaluation before puncture to minimize the occurrence of adverse conditions such as insufficient sample acquisition, diluted blood cells caused by bleeding at the puncture site, and failure of puncture to reach the lesion site, thereby improving the effectiveness, accuracy, and safety of US-FNAC.
There are some limitations in this study. First, among patients undergoing US-FNAC, most patients with malignant nodules and few patients with benign nodules will receive surgical treatment, so selection bias occurred. Second, this single-center study had small sample numbers, so subsequent studies need to extend the observation time and increase the samples. Finally, the different studies had multiple grouping criteria for nodular size, affecting the study results. Therefore, complete verification should be taken by including more samples and conducting multiple studies to provide more reliable information for clinical work.
SUMMARYUS-FNAC has a high diagnostic efficiency for the pathological properties of thyroid nodules. Whether the nodule diameter has an effect on the accuracy of this method requires more clinical evidence.
AVAILABILITY OF DATA AND MATERIALSThe data that support the findings of this study are available from the corresponding author upon reasonable request.
ABBREVIATIONSUS-FNAC- ultrasound-guided fine-needle aspiration cytology ROC- receiver operator characteristic ATA- American Thyroid Association
AUTHOR CONTRIBUTIONSGX: Interpreted the data and wrote the manuscript; WT: Designed the study; WT and GX: Contributed to writing the manuscript. All authors read and approved the final version of the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
Comments (0)