The zero-profile implant (Zero-P) is accepted for use in anterior cervical fusion for the treatment of degenerative cervical disease. However, evidence pertaining to its efficiency and safety in traumatic cervical injury is largely insufficient. This study aimed to compare the overall outcomes of patients who underwent Zero-P for traumatic cervical disc injury.
MethodsData from a total of 53 consecutive patients who underwent surgery for traumatic or degenerative cervical disc disease using the Zero-P were reviewed. Seventeen patients (group A) had traumatic cervical disc injury and the remaining 36 (group B) had degenerative cervical disc herniation. The fusion and subsidence rates and Cobb angle were measured retrospectively from plain radiographs. The patients’ clinical outcomes were evaluated using the Japanese Orthopedic Association (JOA) score and Odom’s criteria.
ResultsThe C2-7 Cobb and operative segmental angles increased by 3.45±7.61 and 2.94±4.59 in group A; and 2.46±7.31 and 2.88±5.49 in group B over 12 postoperative months, respectively. The subsidence and fusion rate was 35.0% and 95.0% in group A; and 36.6% and 95.1% in group B, respectively. None of the parameters differed significantly between groups. The clinical outcomes were similar in both groups in terms of increasing the JOA score and producing a grade higher than “good” using Odom’s criteria.
ConclusionThe application of Zero-P in patients with traumatic cervical disc injury was found to be acceptable when compared with the clinical and radiological outcomes of degenerative cervical spondylosis.
Key Words: Cervical vertebrae · Spinal cord trauma · Allograft.
INTRODUCTION Anterior cervical decompression and fusion (ACDF) is an effective method for the treatment of traumatic and/or degenerative disc lesion because neurologic compressions usually occur anteriorly. Although various modified techniques of ACDF have been developed since it was first described by Smith and Robinson [15], the outcomes of these procedures remain controversial. Traditionally, iliac bone graft with anterior plating was used for ACDF in order to stabilize the cervical spine and promote bone union [9,10]. Additionally, a stand-alone cage was often used to avoid the donor site morbidity and plate-related complications including esophageal injury, screw pullout, and plate migration that can occur in traditional ACDF [5,6]. The zero-profile interbody fusion device, Zero-P (Synthes GmbH, Oberdorf, Switzerland) was invented to reduce platerelated complications. It consists of an interbody spacer and locking screws that can be fixed in the intervertebral space. It has been shown to provide similar biomechanical stability to the use of a cage and anterior plating system [13]. The same conclusion was drawn from a study involving patients with degenerative pathology, and the Zero-P has been used in ACDF for the treatment of degenerative cervical disease [14]. However, these previous studies did not provide sufficient evidence on the efficiency or safety of Zero-P in traumatic cervical disc injury. There has been only one preliminary study on the outcomes of ACDF using Zero-P in subaxial cervical spine trauma [3].In the present study, we performed a retrospective analysis to compare the clinical and radiologic outcomes achieved with ACDF using Zero-P for traumatic cervical disc injury to those achieved for degenerative cervical spondylosis. In addition, Zero-P was used in selected patients with traumatic injury who had no bony fracture, severe segmental instability, or kyphotic deformity requiring posterior instrumentation.
MATERIALS AND METHODS Patient populationWe retrospectively reviewed data from patients treated for ACDF using the Zero-P in our clinic between January 2013 and December 2016. A total of 53 patients were enrolled in this study. Of the 53 patients, 17 were treated with only Zero-P, i.e., without posterior fixation for traumatic disc injury (group A), and the remaining 36 patients were treated for degenerative disc herniation (group B). Surgical indicated levels were a single segment or skipped two segments (not including contiguous two segments, such as C3/4/5), determined by evaluating the preoperative radiologic pathology and clinical symptoms. Patients who met any of the following criteria were excluded in group A : 1) vertebral body fracture, 2) facet dislocation, and 3) cases requiring posterior decompression and instrumentation, such as severe canal stenosis and kyphotic deformity. In addition, the following criteria were also excluded in group A and B as well : 1) prior cervical spine surgery, 2) autoimmune or metabolic bone disease, and 3) postoperative surgical site infection.
In group A, the presence of a paravertebral ligament injury, prevertebral hemorrhage, facet perch and the score from the Sub-axial Cervical Spine Injury Classification System (SLICS) were further evaluated through medical charts, operation records, and preoperative magnetic resonance imaging (Fig. 1). Surgical techniquesFor ACDF using Zero-P, the patient was placed in the supine position under general anesthesia. Fluoroscopy was used to confirm the target level. A horizontal incision was made along the skin crease in the neck that correlated to the target cervical disc. After removal of the intervertebral disc with a careful endplate preparation, generous decompression of the bilateral neuroforamen was performed. A Kerrison punch and high-speed electric drill were used to decompress the nerve roots by removing the osteophyte overgrowth on the uncovertebral joint and posterior lips of the vertebral body. Extensive saline irrigation was performed during drilling of the osteophytes and milling of the endplates. After sufficient decompression, we applied a Zero-P convex implant and 4 Zero-P screws under intraoperative fluoroscopy. After the release of a Casper distractor, a manual pullout test was conducted to confirm the stability of the segments. A closed system drainage catheter was placed. After surgery, all patients were instructed to wear a Philadelphia neck brace for 4 weeks.
Radiological evaluationRadiological images were assessed pre-operation and at follow-ups that occurred approximately 3, 6, and 12 months postoperatively. The cervical curvature angle, fusion status, and subsidence rate was assessed using cervical X-ray and cervical computed tomography (CT). All radiographic reports were interpreted and measured using PACS system software (INFINITT, Seoul, Korea).
The cervical Cobb angle was measured as the acute angle constructed by the lines running along each inferior vertebral endplate of the C2 and C7 vertebral bodies on lateral X-ray. The operative segmental angle was measured as the acute angle constructed by the lines running along the superior and inferior vertebral endplates of the operated vertebral body. The difference between the pre-operative and 12-month postoperative follow-up angles for each parameter was designated as the delta (Δ) value (Fig. 2). The evaluation of fusion of the operated cervical vertebral body was determined using dynamic cervical X-ray 12 months postoperatively. In cases in which it was difficult to determine the fusion status accurately by plain radiograph, the trabecular bone bridge was checked using cervical CT (Fig. 3). The protocol for bone fusion was as follows : 1) magnify image >150%; 2) assess for adequate flexion-extension effort by confirming that there is >4 mm of inter-spinous process motion at a non-arthrodesed level; and 3) ensure there is 17].Cage subsidence was defined as a decrease in interbody height >3 mm on a plain radiograph 12 months postoperatively. The difference in subsidence was based on the length between the center of the upper and lower endplates in a lateral X-ray.
Clinical evaluation The clinical outcomes were evaluated pre- and postoperatively and at the last follow-up using the Japanese Orthopedic Association (JOA) score. At the last follow-up, patients were assessed according to Odom’s criteria, which ranging from ratings of excellent to poor [12]. Statistical analysisPatient characteristics and clinical outcomes were assessed using descriptive analyses, with the mean (standard deviation) and median (interquartile range) presented for quantitative variables and the frequency (percent) presented for qualitative variables. The comparison of characteristics and clinical outcomes between groups A and B were analyzed using twosample t-tests or Mann-Whitney U tests for quantitative variables and chi-square tests or Fisher’s exact test for qualitative variables. p-values are presented for all statistically significant variables. All statistical analyses were performed using the SPSS software package for Windows version 19.0 (IBM, Chicago, IL, USA). All tests were 2-sided, and p-values <0.05 were considered to indicate statistical significance.
RESULTSDemographic data of the patients enrolled in the study
A total of 53 patients who underwent fusion using a Zero-P were enrolled in the study. Group A consisted of 16 men and one woman (mean age, 53.9 years). During the same period, 17 men and 19 women (mean age, 57.0 years) were enrolled in group B (Table 1). In group A, all patients had an interspinous ligament injury, and the incidence of anterior longitudinal ligament injury was higher than that of posterior longitudinal ligament injury. Prevertebral hemorrhage was observed in all patients except one, facet perch was observed in only two patients, and cord signal change was observed in 14 patients (14/17, 76.5%). The SLICS score was at least four points in group A, with five points occurring most frequently. Other detailed data for group A are presented in Table 2. Radiological outcomes The fusion rate was 95.0% (19/20) in group A and 95.1% (39/41) in group B. The mean Cobb and operative segmental angles increased by 3.45 mm and 2.94 mm, respectively, over the preoperative value in group A. Similarly, the Cobb and operative segmental angles increased by 2.46 mm and 2.88 mm, respectively, in group B. Cage subsidence occurred in 7 levels (7/20, 35.0%) in group A and 12 levels (12/41, 29.3%) in group B. None of the measured values were significantly different between the two groups (all p>0.05, Table 3). Clinical outcomes stratified by JOA score and Odom’s criteria Both groups exhibited an improvement in clinical outcomes as demonstrated by the increase from the mean preoperative JOA score to the postoperative JOA scores (JOA; group A, 1.59 ±1.58; group B, 1.44±1.05). There were no statistically significant differences with regard to the JOA values between the two groups (p=0.696). According to Odom’s criteria, all outcomes had a grade higher than “good” in both groups. There vwere no significant differences in the proportions of “good” outcomes between the two groups (p=0.667, Table 4). Comparisons of radiologic and clinical outcomes in male patients We performed a comparative analysis of male subjects in both groups, because group A was mostly consisted of male patients (16/17, 94.1%) and the number was similar to male patients in group B. In terms of radiologic and clinical outcomes, there were no significant differences between male subjects of group A and B. Detailed data for comparisons of both groups are presented in Table 5. ComplicationsThree patients (two in group A and one in group B) suffered from transient dysphagia, but recovered within 3 weeks postoperation. In group B, one patient reported prolonged vocal cord paralysis. No complications requiring re-operation, such as surgical site infection, instrumental failure, or postoperative hematoma, occurred.
DISCUSSION Traumatic cervical injury is a common problem in adults and has a male predominance. The purpose of surgical treatment is the prevention of additional functional loss, the maintenance of neurological function, and the restoration of spinal stability with bone union [1,7]. ACDF with or without posterior fixation has become the most suitable surgery for traumatic cervical injury. The rationale for the use of the cage-plate system in ACDF is that patients who undergo these implants are more likely to require only minimal external bracing and return to normal activities earlier than those who undergo cervical fusion surgery without plating. There are also theoretical benefits, such as initial stability, improved bone fusion, prevention of bone graft collapse, or extrusion and maintenance of sagittal alignment. However, plate-related complications, such as esophagus injury and postoperative dysphagia, can occur [8,18]. Zero-P implants feature a design that fixes the existing stand-alone cage onto the vertebral body with a screw, thereby reducing plate-related complications. Many studies have evaluated the efficacy and safety of the Zero-P implant. Barbagallo et al. found that the Zero-P was associated with good clinical outcomes, such as low rates of neck disability, postoperative dysphagia, and fusion time [2]. Additionally, Njoku et al. [11] reported that the Zero-P had clinical outcomes and radiologic fusion rates comparable with the cage-plate system. Most studies have assessed the postoperative outcomes of ACDF using Zero-P in cases of degenerative cervical spondylosis, Zero-P has been accepted as a useful graft for ACDF in degenerative cervical disc disease [2,4,11,14,16]. Based on these previous studies, we used Zero-P as a graft for ACDF in cases of traumatic disc injury. In the present study, Zero-P was used in selected patients with traumatic injury who had no bony fracture, severe segmental instability, or kyphotic deformity requiring posterior instrumentation. A major concern of ACDF using Zero-P in traumatic injury is the risk of cage subsidence, pseudoarthrosis, and sagittal malalignment. In our series, we focused on objectively comparing these values. The subsidence rate of patients with traumatic injury (group A) was 35.0%, which was similar to the subsidence rate of degenerative spondylosis patients (group B, 29.3%). The fusion rate was 95.0% in group A and 95.1% in group B, and there were few differences between the two groups. In addition, sagittal alignment, including the Cobb angle and the segmental angle, was well maintained postoperatively. Although the number of enrolled patients was small, similar radiologic outcomes were obtained in a study of ACDF using Zero-P in 12 patients with subaxial cervical spine trauma (fusion rate, 100%; no sagittal malalignment) [3].Clinical outcomes such as neck and radicular pain, as well as other neurologic deficits, were alleviated when compared to the patients’ preoperative symptoms 12 months postoperatively. The increase in JOA scores and the proportion of grades higher than “good” using Odom’s criteria were similar in both groups. In addition, the number of patients who suffered from plate-related complications was very low in both groups.
However, we acknowledge the following limitations to our study : 1) the number of patients in the traumatic injury (group A) was relatively small; 2) the follow-up period was relatively short; 3) biomechanical testing was lacking; and 4) the limited inclusion criteria applied to the traumatic injury group were often very subjective and are not backed by scientific literature. Nevertheless, we observed similar fusion and subsidence rates in both groups along with correct sagittal alignment. Clinically, most of the patients (from either group) with neurologic deficit and pain improved after surgery. Finally, we had no patients with chronic dysphagia. Though there were some limitations to our study, we believe that our case series supports the initiation of prospective trials involving multiple centers, larger patient populations, and longer follow-up periods.
CONCLUSIONBased on the results of our study, the overall outcomes achieved for ACDF using Zero-P in cases of traumatic injury were satisfactory and comparable to those achieved in cases of degenerative spondylosis. Therefore, Zero-P implantation in selected patients may be a useful alternative graft option for ACDF in traumatic disc injury.
Fig. 1.Magnetic resonance imaging of the patients revealed the type of associated traumatic cervical injury : a) prevertebral hemorrhage; b) signal change of the cervical cord; and c) suspicious injury of the interspinous ligament.
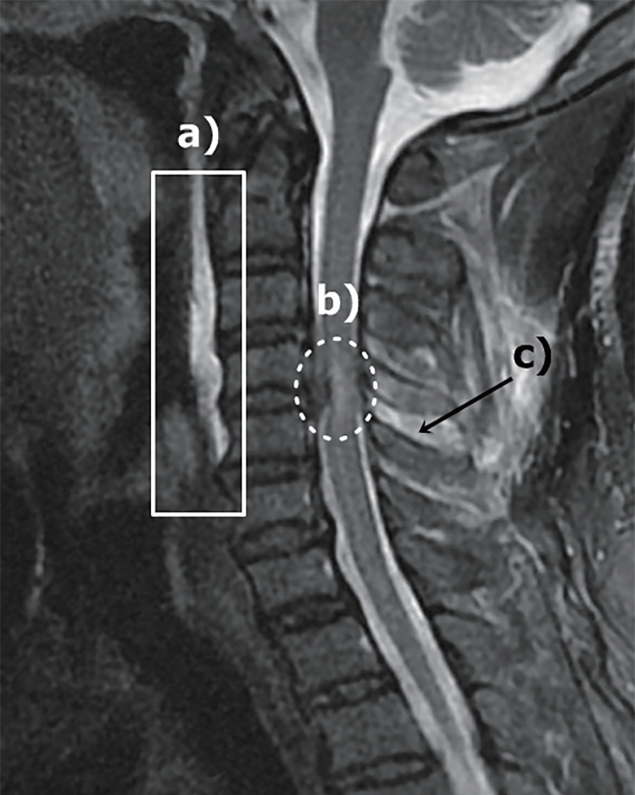 Fig. 2.
Fig. 2.
Measurement of the cervical sagittal alignment : a) operative segmental angle; b) Cobb’s angle.
 Fig. 3.
Fig. 3.
Computed tomography showed additional new bone formation with bony bridging across the disc space.
 Table 1.
Table 1.
Demographic data of the study population
Group A Group B p-value Patients 17 36 Operated level 20 41 0.929* 1 level 14 31 Skipped 2 levels 3 5 Sex 0.001† Male 16 17 Female 1 19 Age (years) 53.9 57 0.432‡ Mean follow-up period (months) 21.6 19.6 0.701‡ Table 2.Detailed demographic data of the patients with traumatic disc injury (group A)
No Sex/age (years) Levels Ligament injury Facet perch Prevertebral hemorrhage Cord signal change SLIC score JOA score ALL PLL ISL 1 M/46 C5-6 X X O X O O 5 16 2 M/53 C3-4/5-6 X X O X O O 5 11 3 M/45 C5-6 O X O O O O 6 9 4 F/76 C5-6 X O O X O O 5 13 5 M/61 C6-7 O X O X O X 5 11 6 M/44 C6-7 O X O X O X 5 16 7 M/22 C3-4 O X O X O X 5 15 8 M/60 C3-4 O O O X O O 5 14 9 M/54 C5-6 O X O X O X 5 16 10 M/51 C3-4 X X O X O O 5 14 11 M/42 C3-4/5-6 X X O X O O 5 9 12 M/58 C6-7 X X O X X O 5 14 13 M/72 C5-6 O X O X O O 6 10 14 M/45 C3-4/5-6 O X O X O O 5 9 15 M/61 C4-5 O X O X O O 4 6 16 M/53 C4-5 O X O O O O 6 15 17 M/73 C6-7 O O O X O O 4 16 Table 3.Comparisons of radiologic outcomes stratified by cervical plain radiographs
Group A (levels, 20) Group B (levels, 41) p-value Operated level C3/4 6 8 0.360* C4/5 2 8 0.346* C5/6 8 22 0.316† C6/7 4 3 0.145* Fusion 19/20 (95.0) 39/41 (95.1) 0.984* ΔC2-C7 Cobb angle (°) 3.45±7.61 2.46±7.31 0987‡ ΔOperative segmental angle (°) 2.94±4.59 2.88±5.49 0.072§ Subsidence 7/20 (35.0) 12/41 (29.3) 0.650† Table 4.Comparisons of clinical outcomes stratified by JOA and Odom’s criteria
Group A (n=7) Group B (n=36) p-value ΔJOA 1.59±1.58 1.44±1.05 0.696* Odom's criteria Excellent 3 12 Good 11 20 Fair 3 3 Poor 0 1 Success ratio 14/17 (82.4) 32/36 (88.89) 0.512† Table 5.Comparisons of radiologic and clinical outcomes in male patients
Males in group A (n=16, levels=19) Males in group B (n=17, levels=20) p-value Fusion 18/19 (94.7) 19/20 (95.0) 0.970* ΔC2-C7 Cobb angle (°) 3.41±7.52 2.21±7.12 0.830† ΔOperative segmental angle (°) 2.82±4.43 2.61±4.93 0.082† Subsidence 7/19 (36.8) 5/20 (25.0) 0.423‡ ΔJOA 1.55±1.56 1.53±1.17
Comments (0)