Intellectual and developmental disabilities (IDD), which affect approximately 1–3% of the general population (1), are characterized by arrested or incomplete development of cognitive, language, motor, and social abilities during the developmental period (2). Individuals with IDD engage in significantly less physical activity (PA) compared to their non-disabled peers, raising serious health concerns (3, 4). Obesity and overweight rates are notably among students with IDD, which can lead to decreased cardiovascular function, disruptions in glucose and lipid metabolism, and increased susceptibility to various chronic diseases (5–8), ultimately impacting overall health into adulthood. Furthermore, limited PA has been associated with poorer mental health outcomes, including higher levels of anxiety and depression (9, 10).
The World Health Organization (WHO) recommended that engaging in 150–300 min of moderate-intensity or 75–150 min of vigorous-intensity PA weekly can effectively prevent cardiovascular diseases and enhance the quality of life (QoL) for individuals with IDD (11). However, students with IDD tend to show a progressive decline in PA and an increase in sedentary behavior as they age, compared to their neurotypical peers (12, 13). This trend may be attributed to various barriers to PA participation, including limited access to sports facilities, insufficient knowledge about available activities, the unique nature of their disabilities, and a lack of support from families and communities (14–16). This unique context necessitates more structured interventions that emphasize motivational support. While school-based interventions for PA are frequently employed in research to improve PA levels and health outcomes, concerns have been raised regarding their effectiveness in achieving meaningful changes in overall PA levels (17, 18). Addressing these clinical conditions requires more than just a school-based approach; the development of healthy behaviors also depends on ongoing parental support and a conducive extracurricular environment.
Parents, motivated by their commitment to their children’s well-being, play a crucial role in providing essential daily support that facilitates sustained participation in positive health behaviors (19). Research indicates that among children with IDD, greater parental support is significantly associated with increased levels of PA reported by parents or caregivers (20, 21). Such support not only shapes children’s PA behaviors but also cultivates a home environment that encourages engagement in PA (22). However, studies exploring the impact of family support on improving PA and subsequent quality of life for children with IDD remain limited. This gap may stem from the challenges associated with implementing effective interventions. Parents often lack the specialized knowledge and strategies needed to address the unique behavioral changes of children with IDD, which can hinder the sustainability of these interventions. Nevertheless, advancements in technology have made it possible to deliver many traditionally in-person services through remote video consultations (23). This shift presents new opportunities to enhance support and engagement in these interventions.
Therefore, the aim of this study is to explore a novel remote collaboration-based family PA intervention to assess its effectiveness in improving PA levels and QoL among children with IDD. Based on this premise, the study proposes the following hypotheses: (1) Remote collaboration-based family PA will effectively enhance PA and QoL in children with IDD; (2) This program will positively influence the maintenance of long-term healthy behaviors among children with IDD. (3) Relying solely on school-based physical activities provides limited benefits for children.
2 Methods 2.1 Study designThis 6-month trial was conducted from September 2023 to February 2024 and included three assessment points: pre-intervention, 6 months post-intervention, and 2 months after the intervention concluded. The first 2 weeks served as an adaptation period to enhance comfort and confidence among participants with IDD (24). To determine the necessary sample size for statistical significance, a significance level of 0.05 and an 80% power requirement indicated that at least 14 participants per group were needed. Considering a potential dropout rate of 10% among students with IDD, a minimum of 32 participants was required to ensure reliable results. This randomized controlled trial (Clinical Registration: NCT06444659) was approved by the Ethics Committee of Hunan Normal University (Approval No. 301, 08/05/2023) and conducted in accordance with the Declaration of Helsinki.
2.2 ParticipantsForty participants were recruited from a specialized school in Changsha, with recruitment and eligibility screening conducted by the school’s physical education teachers. Inclusion criteria consisted of: (1) a diagnosis of mild to moderate intellectual disability (ID) (IQ range: 35–69); (2) age between 14 and 17 years; and (3) at least one family member capable of effective communication with the researchers. Exclusion criteria included: (1) the presence of severe physical disabilities or medical conditions that contraindicate PA, such as severe cardiovascular disease; (2) participation in other exercise programs within the preceding 3 months to mitigate prior PA exposure that could confound the results; and (3) missing more than three intervention sessions to ensure the consistency and reliability of the intervention outcomes.
2.3 InterventionAccording to Figure 1, both the intervention and control groups (CG) participated in physical education classes three times per week. To ensure consistency and further investigate the impact of the school-based exercise intervention on the PA levels of children with IDD, the curriculum content underwent specific adaptations. These adaptations included lowering the difficulty level, enhancing teaching strategies through clear language, goal orientation, and visual support, as well as optimizing the instructional content by incorporating games and team activities. These changes were generally considered effective in promoting participation among individuals with IDD (25, 26). Participants in the CG did not receive additional support from the research team, while those in the Intervention Group (IG) received regular remote support as follows:
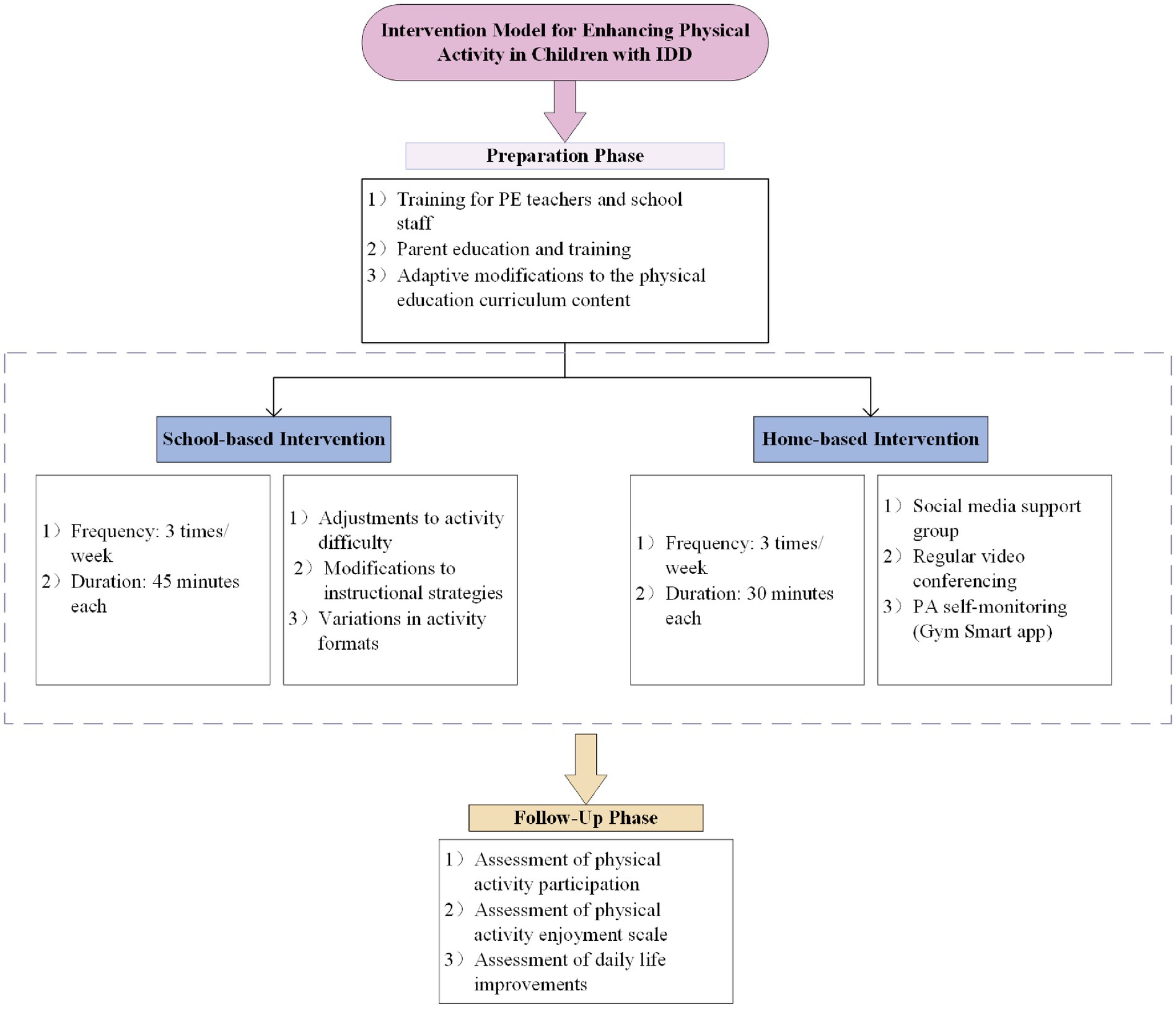
Figure 1. Model of the physical activity intervention.
Before the intervention, all parents received comprehensive PA education and training from experts in education, sports, and health to effectively support their children. Additionally, remote collaborative family PA sessions were conducted via Tencent’s VooV Meeting platform, comprising three 30-min meetings each week. The team consisted of a special education expert and a professor with experience in promoting PA among children. Due to the varying circumstances of each family, the curriculum content was not strictly prescribed; instead, activities were selected based on what children with IDD could accomplish and were willing to engage in, such as various ball games, jump rope, and jogging. Parents utilized video check-ins to ensure the proper implementation of personalized routines, while the Gym Smart (V 1.0; Gezhi Technology, Chengdu, China) was employed to monitor exercise intensity in real time, ensuring safety and facilitating necessary adjustments.
2.4 MeasuresTo evaluate baseline and 6-month PA levels in individuals with IDD, we employed ActiGraph GT3X+ (ActiGraph LLC, Pensacola, FL) triaxial accelerometers. The effectiveness of ActiGraphs in measuring PA levels among IDD students was validated (27, 28). Prior to testing, parents and teachers received training on the proper placement of the accelerometer on the right hip joint (29). IDD students wore the accelerometer continuously for 7 days (5 weekdays and 2 weekends) (30), Removing it only during bathing and sleeping, researchers contacted parents daily to ensure compliance and inquired about accelerometer wear. Real-time supervision occurred during school hours. We applied Choi’s criteria for accelerometer valid data selection to calculate wearing and non-wearing times (31). In line with Chinese adolescent and children’s PA recommendations (32), the accelerometer sampling interval was set at 1 s with a frequency of 60 Hz. Light physical activity (LPA) was defined as 100 to 2,799 counts per minute (CPM), while moderate-to-vigorous physical activity (MVPA) was classified as activity intensity exceeding 2,800 CPM. Assessments were conducted before the intervention, after the intervention, and at a 2-month follow-up following the trial’s conclusion.
Considering the subjective experiences of children with IDD, the WHOQOL-DIS-ID scale was selected to assess their QoL (33). Numerous studies have established its validity and reliability (34, 35). Participants responded to 12 items, each offering five possible answers.
The Physical Activity Enjoyment Scale (PACES) (36) is used to assess enjoyment of PA and has been proven to be reliable and valid. The questionnaire consists of 16 questions rated on a 5-point scale. The scale consists of 9 positively worded items and 7 negatively worded items. Scores for the 7 negatively worded items are reverse-coded and then combined with the scores for the positively worded items. Higher total scores indicate greater levels of enjoyment.
2.5 Statistical analysesAll statistical analyses were performed using SPSS version 23.0. Data are presented as mean ± standard deviation (M ± SD). The Shapiro–Wilk test was used to assess the normality of the data distribution. For normally distributed data, paired sample t-tests were conducted to evaluate within-group changes. For non-normally distributed data, the Wilcoxon signed-rank test was employed. Accelerometer data, including sedentary time and MVPA, as well as QoL scores, were analyzed using repeated measures ANOVA. Post-hoc analyses were conducted in instances of significant findings. Greenhouse–Geisser correction was applied when the assumption of sphericity was violated.
3 Results 3.1 Participant characteristicsAs shown in the flow chart (Figure 2), among the 40 participants, 4 withdrew during the intervention: 2 due to lack of effective support from guardians for family reasons, and 2 in the later stages of the trial due to an inability to continue with follow-up tests after contracting influenza.
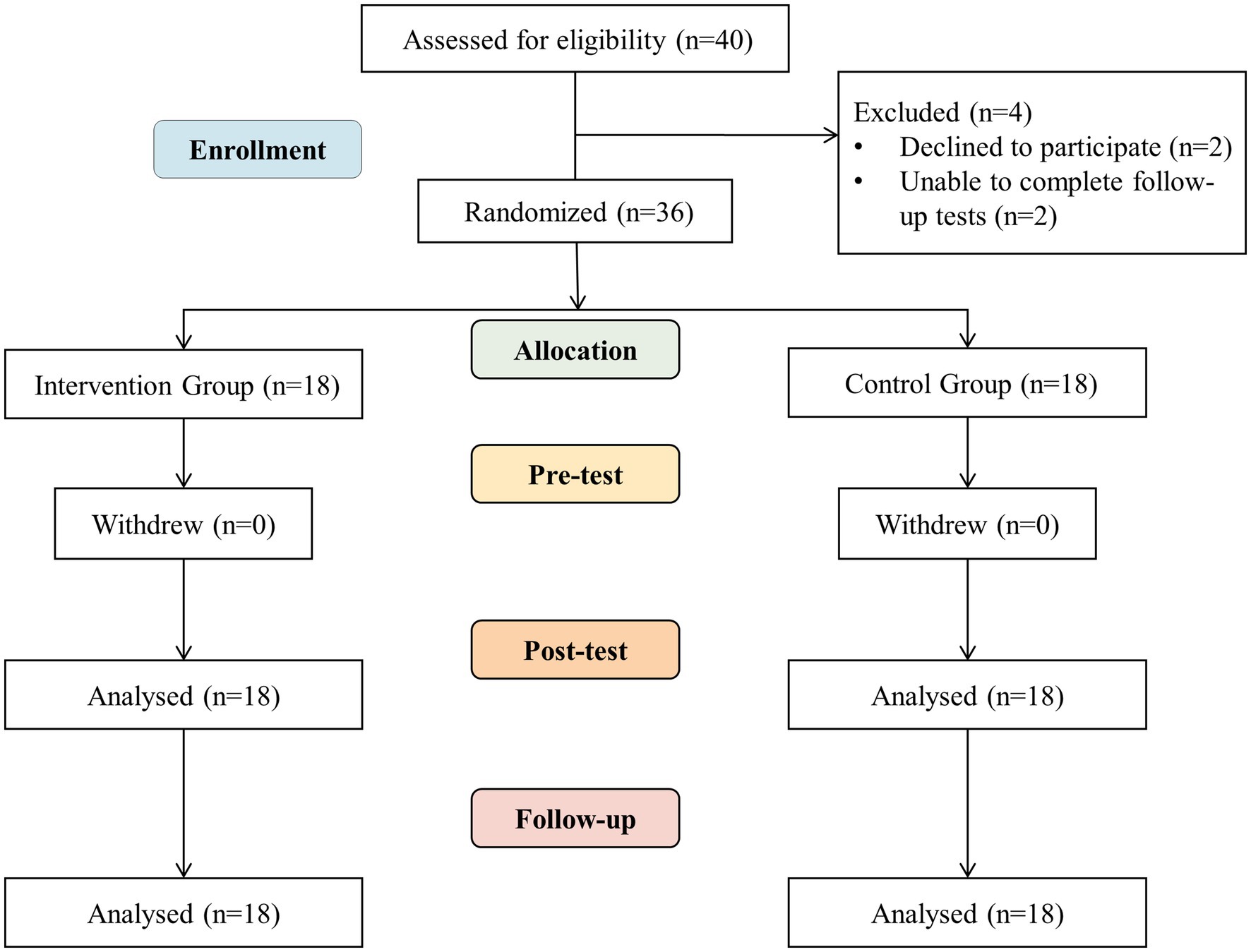
Figure 2. Study flow chart.
A total of 36 participants completed the trial, with 58.3% being male and 41.7% female, and an average age of 16.44 years (± 0.73). Among these participants, 23 were diagnosed with mild intellectual disabilities, while 13 were classified with moderate intellectual disabilities. The cohort also included four students with Down syndrome and three students on the autism spectrum. Additionally, one participant designated their sister as the primary contact for the study due to parental circumstances (see Table 1).
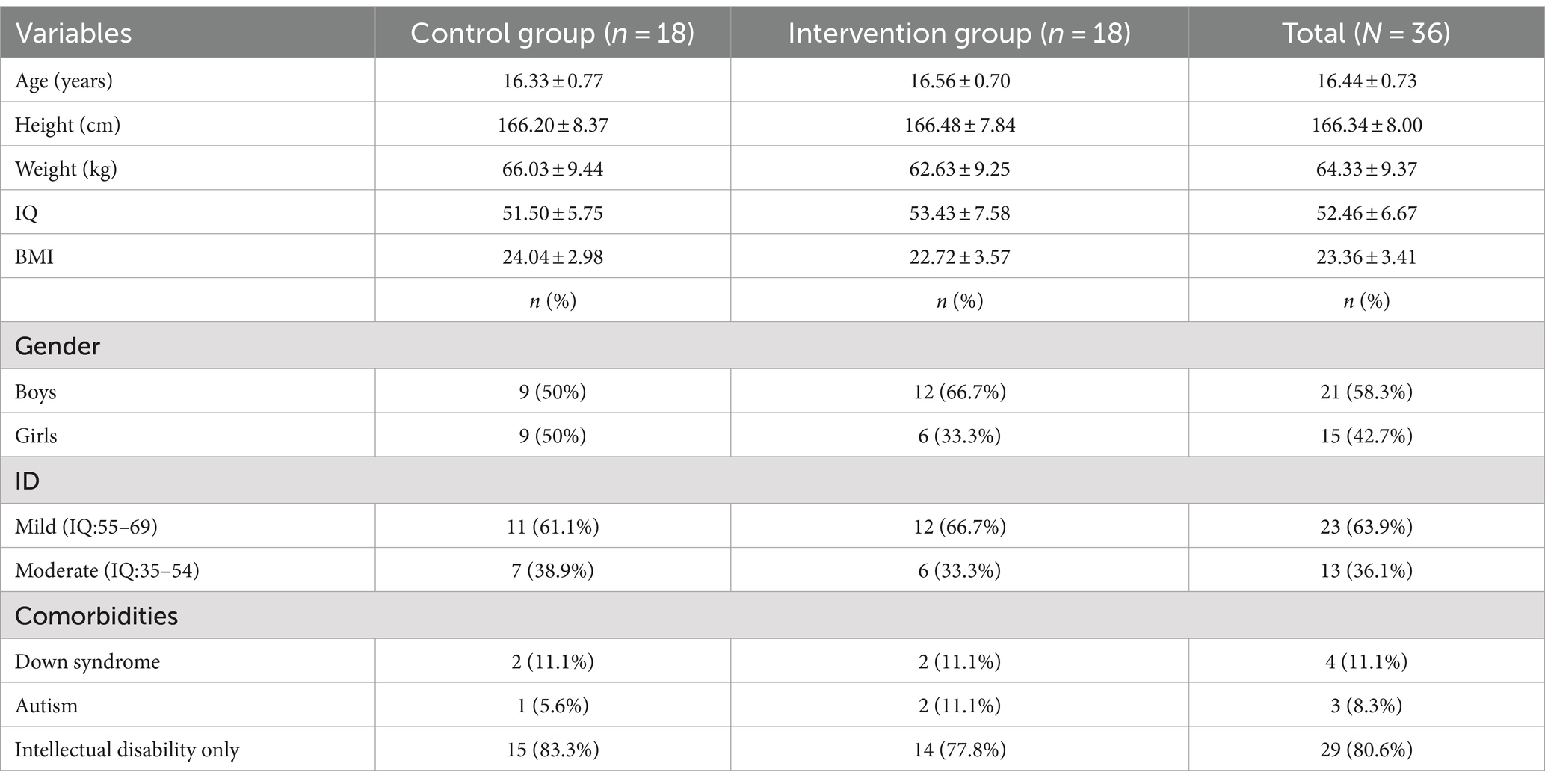
Table 1. Descriptive characteristics of participants.
3.2 Primary outcomeFigure 3 displays the health outcomes of participants in both the IG and CG over a 6-month period, with assessments at T1 (pre-intervention), T2 (6 months post-intervention), and T3 (2-month follow-up). The findings reveal that modifications to the physical education curriculum in the CG did not result in meaningful changes in MVPA, sedentary behavior, QoL scores, or PACES assessments. Conversely, the IG exhibited a noteworthy increase of 19.1 min in MVPA and a reduction of 56.34 min in sedentary time following the intervention. Furthermore, improvements were noted in QoL, with WHOQOL-DIS-ID scores rising by 5.05, and PACES scores increasing by 7.12, all with p-values below 0.001.
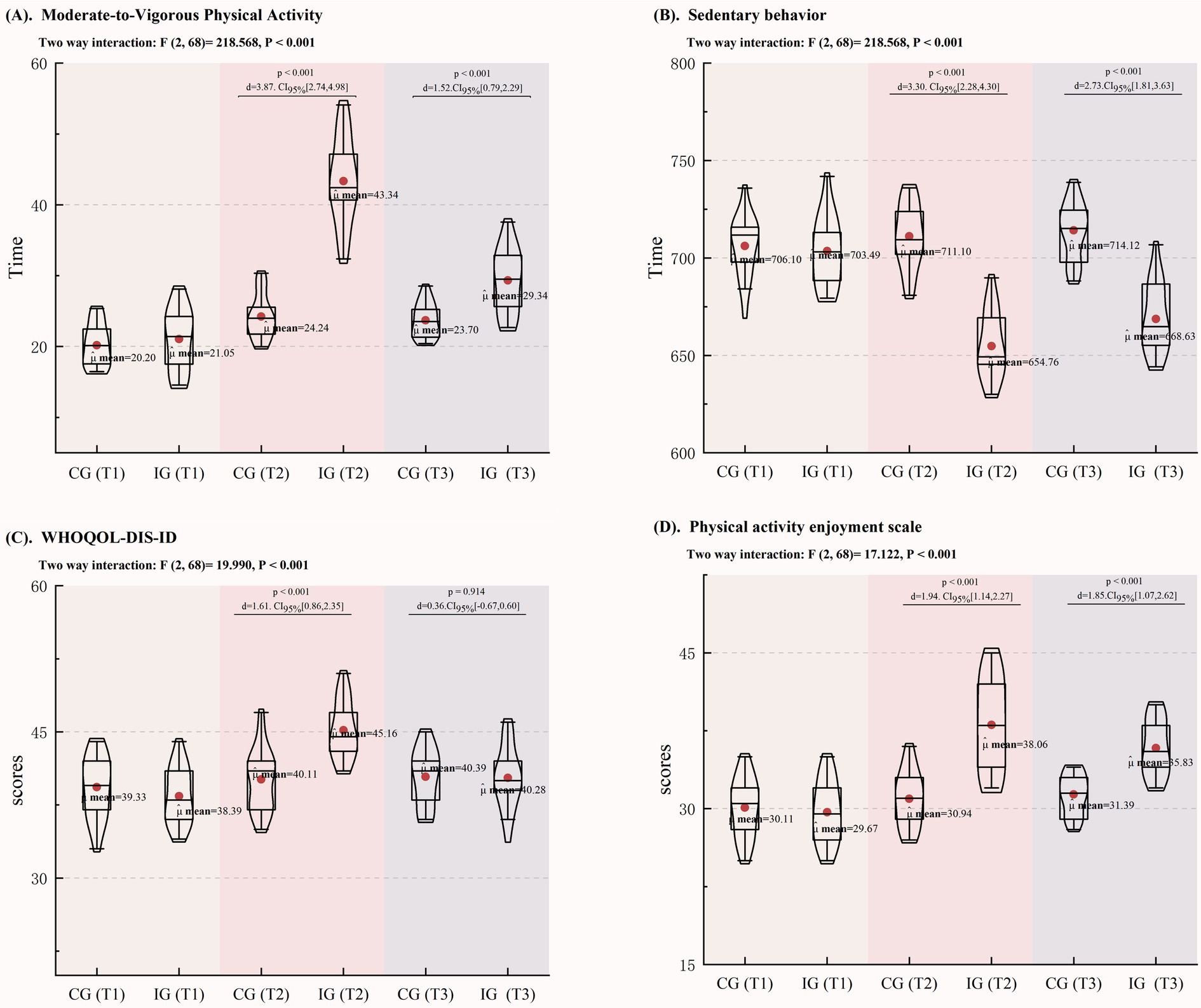
Figure 3. Changes in PA, WHOQoL-DIS, and PACES among Children with IDD. (A) Changes in MVPA; (B) Changes in Sedentary Behavior; (C) Changes in the WHOQoL-DIS-ID; (D) Changes in the PACES.
At the 2-month follow-up (T3), while some metrics in the IG showed a decline, participants still engaged in 5.64 more minutes of MVPA and reduced sedentary behavior by 15.49 min compared to the CG. Additionally, PACES scores remained 4.44 points higher in the IG, with p-values consistently below 0.001. These results suggest that the intervention may promote the development of long-term healthy behaviors among children with IDD, despite no significant change in WHOQOL-DIS-ID scores (p = 0.914).
4 DiscussionNumerous studies have established the pivotal role of parental support in fostering the healthy development of children with IDD (37–39). However, translating this support into practical applications presents significant challenges. This research offers the first empirical evidence highlighting the importance of remote collaborative family activities in sustaining long-term healthy behaviors among children with IDD, thereby enhancing the existing body of literature. Our approach uniquely combines an online platform with a family-oriented PA program, delivering real-time feedback and personalized support tailored to the specific needs of each child. This innovative integration not only encourages active parental engagement, thereby strengthening their role in promoting their children’s health behaviors, but also effectively mitigates barriers that traditional school-based methods may overlook. In comparison to broader school interventions, this model provides a more comprehensive and adaptable strategy for maintaining behavioral change, emphasizing the crucial involvement of families in supporting the health and well-being of children.
Regular participation in physical activity offers numerous lifelong benefits. However, children with IDD face multiple barriers that hinder their engagement and maintenance of physical activity (40, 41), with the role of parents being particularly significant (38, 42). Common obstacles include a lack of parental support, excessive vigilance and protection, and insufficient knowledge about physical activity (43, 44). Addressing these barriers should be a primary focus in promoting physical activity among children with IDD. Parents play an essential role by creating a supportive activity environment, providing emotional encouragement, and instilling healthy values (14, 43). Our findings provide empirical support for this perspective and offer new insights for designing physical activity programs that support parents. Specifically, a family-based activity model facilitated through remote collaboration effectively addresses these challenges, presenting new opportunities for enhancing the health behaviors of children with IDD.
Multiple studies have demonstrated that structured school-based PA positively impacts the health of children with IDD, such as Wang’s 12-week school-based physical intervention, which effectively improved obesity and health-related physical fitness (HRPF) in children with IDD (45). Despite these benefits, children with IDD face various limitations to participation, raising questions about whether school-based activities alone can enhance their PA levels and foster long-term healthy behaviors (18, 52). Our findings support this concern, as the control group showed no significant improvement in physical activity levels, even with some adaptations to the physical education curriculum. When promoting physical activity for children with IDD, it is essential to consider individual factors such as physical skills, cognitive abilities, and self-efficacy, alongside interpersonal influences from teachers, peers, and parents, as well as environmental constraints like community resources and weather conditions (20, 46–48). While existing research underscores the role of physical education classes and recess in facilitating MVPA for children with IDD (49), our results indicate that relying solely on school-based activities may yield limited benefits and fail to sustain long-term healthy behaviors. Therefore, future research should explore the diverse barriers and facilitators influencing participation in physical activity among children with IDD. A focus on parental education and strategies to enhance children’s ongoing engagement will be crucial for fostering sustained behavioral improvements in this population.
The results of the 6-month intervention revealed significant improvements in the PA levels of children with IDD, accompanied by a reduction in sedentary behavior and positive effects on their QoL. Most studies have confirmed that improvements in QoL are closely associated with increased PA (50, 51). This study not only corroborates this relationship but also suggests that this perspective can be extended to the IDD population. The follow-up assessment conducted 2 months later further validated our hypothesis that incorporating family-based physical activities as a supplement to extracurricular activities not only enhances children’s well-being but also fosters the potential for them to maintain active lifestyles and continue engaging in physical activities in the future.
In summary, family-based PA facilitated through remote collaboration offers new insights for promoting the overall well-being of children with IDD. This approach enhances parental involvement in their children’s PA, thereby supporting the maintenance of long-term healthy behaviors. Furthermore, we anticipate that the application of this method will extend beyond improving the QoL for individuals with IDD, potentially benefiting other disability groups that require personalized exercise interventions.
5 Study limitationsWhile this study provides valuable insights, it is important to acknowledge several limitations. First, the relatively small sample size may restrict the generalizability and applicability of the findings. Second, the potential variability in family engagement is a significant limitation, as differences in parental availability, motivation, and understanding of the intervention may affect the consistency and effectiveness of participation in the family-based activities. Future research should address these gaps to better inform the development of tailored programs for children with IDD.
6 ConclusionFamily-based physical activities facilitated through remote collaboration have proven effective in improving the PA levels and QoL of children with IDD. This model offers new insights into how to develop exercise programs that actively involve parents and provides empirical evidence to support this approach. Furthermore, the findings underscore the challenges associated with relying solely on school-based physical activities to enhance participation among children with IDD, indicating a need for more targeted and motivationally engaging structured activities.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Ethics Committee of Hunan Normal University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributionsXS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. PH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Writing – original draft. MS: Conceptualization, Investigation, Methodology, Project administration, Writing – review & editing. ZL: Formal analysis, Investigation, Writing – review & editing. QL: Writing – review & editing. YG: Formal analysis, Funding acquisition, Investigation, Project administration, Supervision, Visualization, Writing – review & editing, Conceptualization, Data curation, Methodology, Resources, Software, Validation. LZ: Writing – review & editing.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was funded by the Scientific Research Project of the Hunan Provincial Department of Education (Grant No. 23B0079) and the Hunan Province College Students Innovation and Entrepreneurship Training Program (Grant No. S202310542105).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Harris, JC. Intellectual disability: Understanding its development, causes, classification, evaluation, and treatment. Oxford: Oxford University Press (2006).
2. World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization (1992).
3. Frey, GC, Stanish, HI, and Temple, VA. Physical activity of youth with intellectual disability: review and research agenda. Adapt Phys Act Q. (2008) 25:95–117. doi: 10.1123/apaq.25.2.95
PubMed Abstract | Crossref Full Text | Google Scholar
4. Phillips, AC, and Holland, AJ. Assessment of objectively measured physical activity levels in individuals with intellectual disabilities with and without Down’s syndrome. PLoS One. (2011) 6:e28618. doi: 10.1371/journal.pone.0028618
PubMed Abstract | Crossref Full Text | Google Scholar
6. Rimmer, J, Yamaki, K, Lowry, BMD, Wang, E, and Vogel, LC. Obesity and obesity-related secondary conditions in adolescents with intellectual/developmental disabilities. J Intellect Disabil Res. (2010) 54:787–94. doi: 10.1111/j.1365-2788.2010.01305.x
PubMed Abstract | Crossref Full Text | Google Scholar
8. Emerson, E, Hatton, C, Baines, S, and Robertson, J. The physical health of British adults with intellectual disability: cross sectional study. Int J Equity Health. (2016) 15:1–9. doi: 10.1186/s12939-016-0296-x
Crossref Full Text | Google Scholar
9. Biddle, SJH, and Asare, M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. (2011) 45:886–95. doi: 10.1136/bjsports-2011-090185
PubMed Abstract | Crossref Full Text | Google Scholar
10. Bell, SL, Audrey, S, Gunnell, D, Cooper, A, and Campbell, R. The relationship between physical activity, mental wellbeing and symptoms of mental health disorder in adolescents: a cohort study. The. Int J Behav Nutr Phys Act. (2019) 16:138. doi: 10.1186/s12966-019-0901-7
PubMed Abstract | Crossref Full Text | Google Scholar
11. Bull, FC, al-Ansari, SS, Biddle, S, Borodulin, K, Buman, MP, Cardon, G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
PubMed Abstract | Crossref Full Text | Google Scholar
12. Carlon, SL, Taylor, NF, Dodd, KJ, and Shields, N. Differences in habitual physical activity levels of young people with cerebral palsy and their typically developing peers: a systematic review. Disabil Rehabil. (2013) 35:647–55. doi: 10.3109/09638288.2012.715721
PubMed Abstract | Crossref Full Text | Google Scholar
13. Borland, R, Hu, N, Tonge, B, Einfeld, S, and Gray, KM. Participation in sport and physical activity in adults with intellectual disabilities. J Intellect Disabil Res. (2020) 64:908–22. doi: 10.1111/jir.12782
PubMed Abstract | Crossref Full Text | Google Scholar
14. Barr, M, and Shields, N. Identifying the barriers and facilitators to participation in physical activity for children with down syndrome. J Intellect Disabil Res. (2011) 55:1020–33. doi: 10.1111/j.1365-2788.2011.01425.x
PubMed Abstract | Crossref Full Text | Google Scholar
15. Njelesani, J, Leckie, K, Drummond, J, and Cameron, D. Parental perceptions of barriers to physical activity in children with developmental disabilities living in Trinidad and Tobago. Disabil Rehabil. (2015) 37:290–5. doi: 10.3109/09638288.2014.918186
PubMed Abstract | Crossref Full Text | Google Scholar
16. Yu, S, Wang, T, Zhong, T, Qian, Y, and Qi, J. Barriers and facilitators of physical activity participation among children and adolescents with intellectual disabilities: a scoping review. Healthcare. (2022) 10:233. doi: 10.3390/healthcare10020233
Crossref Full Text | Google Scholar
17. Wang, A, Gao, Y, Wang, J, Brown, TJ, Sun, Y, Yu, S, et al. Interventions for health-related physical fitness and overweight and obesity in children with intellectual disability: systematic review and meta-analysis. J Appl Res Intellect Disabil. (2022) 35:1073–87. doi: 10.1111/jar.12999
Crossref Full Text | Google Scholar
18. Metcalf, B, Henley, W, and Wilkin, T. Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54). BMJ. (2012) 345:345. doi: 10.1136/bmj.e5888
Crossref Full Text | Google Scholar
19. Khor, SP, McClure, A, Aldridge, G, Bei, B, and Yap, MBH. Modifiable parental factors in adolescent sleep: a systematic review and meta-analysis. Sleep Med Rev. (2021) 56:101408. doi: 10.1016/j.smrv.2020.101408
PubMed Abstract | Crossref Full Text | Google Scholar
20. Pitchford, EA, Siebert, E, Hamm, J, and Yun, J. Parental perceptions of physical activity benefits for youth with developmental disabilities. Am J Intellect Dev Disabil. (2016) 121:25–32. doi: 10.1352/1944-7558-121.1.25
PubMed Abstract | Crossref Full Text | Google Scholar
21. Lin, J-D, Lin, PY, Lin, LP, Chang, YY, Wu, SR, and Wu, JL. Physical activity and its determinants among adolescents with intellectual disabilities. Res Dev Disabil. (2010) 31:263–9. doi: 10.1016/j.ridd.2009.09.015
PubMed Abstract | Crossref Full Text | Google Scholar
22. Edwardson, CL, and Gorely, T. Parental influences on different types and intensities of physical activity in youth: a systematic review. Psychol Sport Exerc. (2010) 11:522–35. doi: 10.1016/j.psychsport.2010.05.001
PubMed Abstract | Crossref Full Text | Google Scholar
24. Skinner, JS. Exercise testing and exercise prescription for special cases: Theoretical basis and clinical application. Philadelphia: Lippincott Williams & Wilkins (2005).
25. Regaïeg, G, Kermarrec, G, and Sahli, S. Designed game situations enhance fundamental movement skills in children with down syndrome. J Intellect Disabil Res. (2020) 64:271–9. doi: 10.1111/jir.12717
PubMed Abstract | Crossref Full Text | Google Scholar
26. Boman, C, and Bernhardsson, S. Exploring needs, barriers, and facilitators for promoting physical activity for children with intellectual developmental disorders: a qualitative focus group study. J Intellect Disabil. (2023) 27:5–23. doi: 10.1177/17446295211064368
PubMed Abstract | Crossref Full Text | Google Scholar
27. McGarty, AM, Penpraze, V, and Melville, CA. Accelerometer use during field-based physical activity research in children and adolescents with intellectual disabilities: a systematic review. Res Dev Disabil. (2014) 35:973–81. doi: 10.1016/j.ridd.2014.02.009
PubMed Abstract | Crossref Full Text | Google Scholar
28. Pan, C-Y, Liu, CW, Chung, IC, and Hsu, PJ. Physical activity levels of adolescents with and without intellectual disabilities during physical education and recess. Res Dev Disabil. (2015) 36:579–86. doi: 10.1016/j.ridd.2014.10.042
PubMed Abstract | Crossref Full Text | Google Scholar
29. Hildebrand, M, van Hees, VT, Hansen, BH, and Ekelund, U. Age group comparability of raw accelerometer output from wrist-and hip-worn monitors. Med Sci Sports Exerc. (2014) 46:1816–24. doi: 10.1249/MSS.0000000000000289
PubMed Abstract | Crossref Full Text | Google Scholar
30. Kang, M, Bjornson, K, Barreira, TV, Ragan, BG, and Song, K. The minimum number of days required to establish reliable physical activity estimates in children aged 2–15 years. Physiol Meas. (2014) 35:2229–37. doi: 10.1088/0967-3334/35/11/2229
PubMed Abstract | Crossref Full Text | Google Scholar
31. CHOI, L, LIU, Z, MATTHEWS, CE, and BUCHOWSKI, MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. (2011) 43:357–64. doi: 10.1249/MSS.0b013e3181ed61a3
PubMed Abstract | Crossref Full Text | Google Scholar
32. Zhu, Z, Tang, Y, Zhuang, J, Liu, Y, Wu, X, Cai, Y, et al. Physical activity, screen viewing time, and overweight/obesity among Chinese children and adolescents: an update from the 2017 physical activity and fitness in China—the youth study. BMC Public Health. (2019) 19:1–8. doi: 10.1186/s12889-019-6515-9
Crossref Full Text | Google Scholar
34. Sorkhi, N, Akbarzade, I, Nedjat, S, Khosravi, M, Nazemipour, M, Memari, AH, et al. Validity and reliability of the persian version of the world health organization quality of life disabilities module. J Intellect Disabil. (2024) 28:240–60. doi: 10.1177/17446295221123867
PubMed Abstract | Crossref Full Text | Google Scholar
35. Bredemeier, J, Wagner, GP, Agranonik, M, Perez, TS, and Fleck, MP. The World Health Organization quality of life instrument for people with intellectual and physical disabilities (WHOQOL-dis): evidence of validity of the Brazilian version. BMC Public Health. (2014) 14:538. doi: 10.1186/1471-2458-14-538
PubMed Abstract | Crossref Full Text | Google Scholar
36. Motl, RW, Dishman, RK, Saunders, R, Dowda, M, Felton, G, and Pate, RR. Measuring enjoyment of physical activity in adolescent girls. Am J Prev Med. (2001) 21:110–7. doi: 10.1016/S0749-3797(01)00326-9
PubMed Abstract | Crossref Full Text | Google Scholar
37. Ku, B, and Rhodes, RE. Physical activity behaviors in parents of children with disabilities: a systematic review. Res Dev Disabil. (2020) 107:103787. doi: 10.1016/j.ridd.2020.103787
PubMed Abstract | Crossref Full Text | Google Scholar
38. McGarty, AM, and Melville, CA. Parental perceptions of facilitators and barriers to physical activity for children with intellectual disabilities: a mixed methods systematic review. Res Dev Disabil. (2018) 73:40–57. doi: 10.1016/j.ridd.2017.12.007
PubMed Abstract | Crossref Full Text | Google Scholar
39. Ku, B, MacDonald, M, Hatfield, B, and Gunter, KB. Parental influences on parent-reported motor skills in young children with developmental disabilities. Disabil Health J. (2020) 13:100910. doi: 10.1016/j.dhjo.2020.100910
PubMed Abstract | Crossref Full Text | Google Scholar
40. Ewing, G, McDermott, S, Thomas-Koger, M, Whitner, W, and Pierce, K. Evaluation of a cardiovascular health program for participants with mental retardation and normal learners. Health Educ Behav. (2004) 31:77–87. doi: 10.1177/1090198103259162
PubMed Abstract | Crossref Full Text | Google Scholar
41. Grandisson, M, Tétreault, S, and Freeman, AR. Enabling integration in sports for adolescents with intellectual disabilities. J Appl Res Intellect Disabil. (2012) 25:217–30. doi: 10.1111/j.1468-3148.2011.00658.x
PubMed Abstract | Crossref Full Text | Google Scholar
42. Shields, N, Synnot, AJ, and Barr, M. Perceived barriers and facilitators to physical activity for children with disability: a systematic review. Br J Sports Med. (2012) 46:989–97. doi: 10.1136/bjsports-2011-090236
PubMed Abstract | Crossref Full Text | Google Scholar
43. Yu, S, et al. Barriers and facilitators of physical activity participation among children and adolescents with intellectual disabilities: a scoping review. Healthcare. (2022) 10:384. doi: 10.3390/healthcare10020384
PubMed Abstract | Crossref Full Text | Google Scholar
44. Stevens, G, Jahoda, A, Matthews, L, Hankey, C, Melville, C, Murray, H, et al. A theory-informed qualitative exploration of social and environmental determinants of physical activity and dietary choices in adolescent
Comments (0)