Biegus J, Voors AA, Collins SP, Kosiborod MN, Teerlink JR, Angermann CE, Tromp J, Ferreira JP, Nassif ME, Psotka MA, Brueckmann M, Salsali A, Blatchford JP, Ponikowski P. (Institute of Heart Diseases, Wroclaw Medical University, ul. Borowska 213, Wroclaw 50-556, Poland; Department of Cardiology, University of Groningen, University Medical Center Groningen, Hanzeplein 1, Groningen, The Netherlands; Department of Emergency Medicine, Vanderbilt University Medical Center, Nashville, Tennessee, USA; Geriatric Research and Education Clinical Care, Tennessee Valley Healthcare Facility VA Medical Center, Nashville, Tennessee, USA; Saint Luke’s Mid America Heart Institute, University of Missouri-Kansas City, Kansas City, Missouri, USA; The George Institute for Global Health and the University of New South Wales, Sydney, New South Wales, Australia; Section of Cardiology, San Francisco Veterans Affairs Medical Center and School of Medicine, University of California San Francisco, San Francisco, California, USA; Comprehensive Heart Failure Center Würzburg, University and University Hospital Würzburg, and Department of Medicine 1, University Hospital Würzburg, Am Schwarzenberg 15, Haus A15 97078 Würzburg, Germany; Saw Swee Hock School of Public Health, National University of Singapore, the National University Health System, Singapore; Université de Lorraine, Inserm, Centre d’Investigations Cliniques Plurithématique 1433, and Inserm U1116, CHRU, F-CRIN INI-CRCT [Cardiovascular and Renal Clinical Trialists], Nancy, France; UnIC@RISE, Department of Surgery and Physiology, Cardiovascular Research and Development Center, University of Porto, Porto, Portugal; Inova Heart and Vascular Institute, Falls Church, Virginia, USA; Boehringer Ingelheim International GmbH, Binger Straße 173, 55216 Ingelheim am Rhein, Germany; First Department of Medicine, Faculty of Medicine Mannheim, University of Heidelberg, Germany; Novo Nordisk Pharmaceutical Company, Copenhagen, Denmark; Faculty of Medicine, Rutgers University, New Brunswick, New Jersey, USA; Elderbrook Solutions GmbH, Sky Tower, Borsigstr. 4, Bietigheim-Bissingen, Germany.) Impact of empagliflozin on decongestion in acute heart failure: The EMPULSE trial. Eur Heart J 2023;44:41–50.
SUMMARYDecongestion is the major goal of treatment in case of acute heart failure (AHF). Usually, diuretics are given in decongestion but this trial aimed to explore the role of SGLT-2 inhibitors such as empagliflozin in controlling decongestion; the underlying mechanism of action of the drug in AHF is still unknown. The trial also sought to establish the effectiveness of SGLT-2 inhibitors in the therapy of AHF.
EMPULSE was an international, multicentre, double-blind, randomized trial aimed at assessing the impact of oral empagliflozin in comparison to a placebo regarding its effects on clinical outcomes, safety and patient tolerability in AHF. The trial was conducted on a total of 530 hospitalized patients with AHF, who after initial stabilization were 1:1 randomized to receive either 10 mg empagliflozin (once daily) or placebo for 90 days. The outcomes investigated were time to all-cause death, number of HF events (including hospitalizations for HF, urgent HF visits and unplanned outpatient visits), time to first HF event, and a ≥5 point difference in change from baseline in the Kansas City Cardiomyopathy Questionnaire total symptom score (KCCQ-TSS) after 90 days of treatment. The additional end-points used in the analysis included weight reduction, weight loss adjusted for the mean daily dose of loop diuretics, the area under the curve (AUC) representing the change in log-transformed N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels over 30 days of treatment, haemoconcentration determined by alterations in haematocrit levels, and a clinical congestion score. The clinical congestion score was computed by summing points assigned to specific signs and symptoms.
The results of the study showed a significantly higher weight loss at days 15, 30 and 90 from baseline with adjusted mean difference as 1.97, 1.74 and 1.53 kg for patients on empagliflozin compared to those on placebo. A significant reduction of NT-proBNP on days 15 and 30 from baseline with adjusted geometric mean ratio as 0.92 and 0.90, respectively, for patients on empagliflozin compared to those on placebo. The haematocrit rose significantly in patients on empagliflozin with the adjusted mean differences as 1.71, 1.62 and 1.94 at days 15, 30 and 90, respectively, compared to those on placebo. Patients on empagliflozin had a significant score reduction with adjusted mean difference as 0.34 on comparison with those on placebo at day 15. Hence, when compared with the placebo group, empagliflozin treatment exhibited a consistent trend of significantly larger alterations in all assessed indicators of decongestion across most time intervals.1
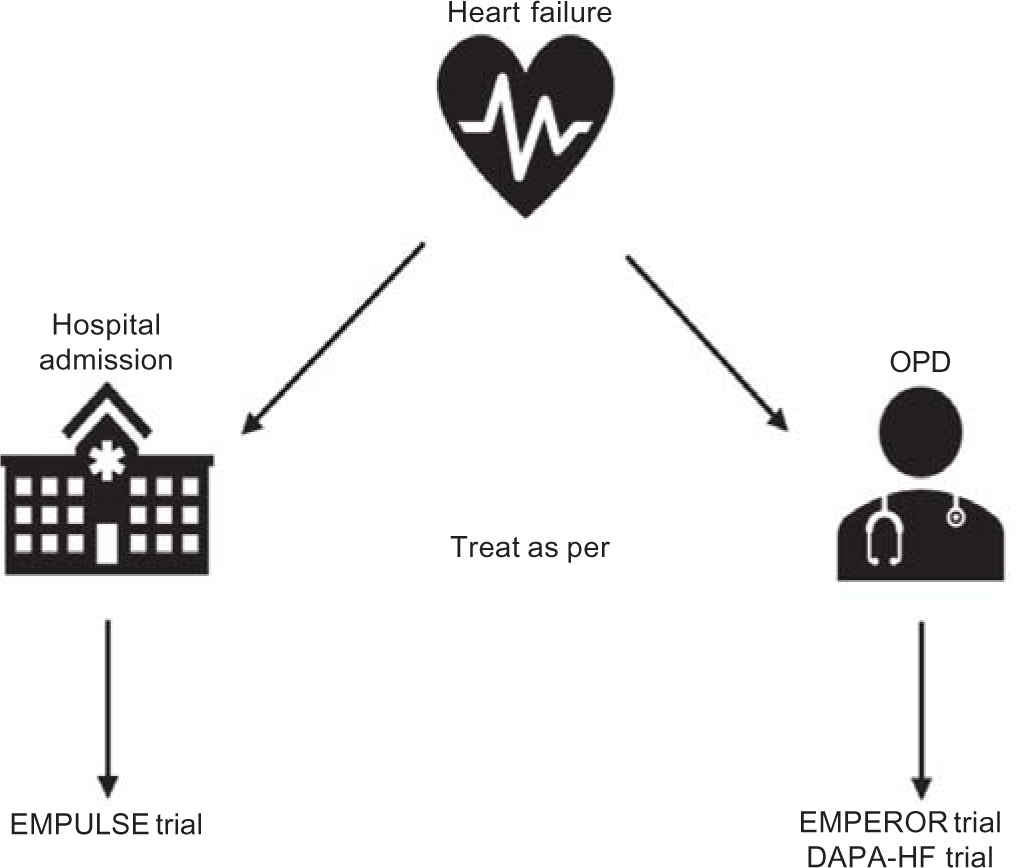
COMMENTSGLT-2 inhibitors are now the standard of care in the management of HF across the spectrum of ejection fraction (EF). Based on the positive results of pivotal trials in HF with reduced EF and HF preserved EF, major guidelines advocate their use in chronic HF therapy in the outpatient setting (Fig. 1).1–3 However, there was dearth of data regarding their use in AHF. The SOLOISTWHF did allow the use of SGLT-2 inhibitor early after discharge but in acute in-hospital phase. The huge morbidity and mortality of AHF represented an unmet need in the pharmacological management of this scenario. Moreover, there are theoretical concerns regarding hypotension, worsening renal function, hypoglycaemia and ketoacidosis early after SGLT-2i initiation, which could be counterproductive with the decompensated haemodynamics seen in AHF. The EMPULSE trial is the first to use SGLT-2 inhibitor in a scenario of AHF and the positive results are a shot in the arm for HF pharmacotherapy in acute settings.
Export to PPT
The EMPULSE study concluded that empagliflozin administration in AHF resulted in early, effective and sustained improvements in all the studied parameters of decongestion such as weight loss, NT-pro-BNP, diuretic dose and clinical congestion score. The study had the following limitations, having a small number of enrolled patients and the use of restrictive inclusion and exclusion criteria, limiting its generalizability. The weight of the patients was not monitored throughout the hospital stay, hindering comparisons with other studies focused on in-hospital decongestion. However, the study did provide valuable insights into the early post-discharge phase of the disease. Mechanistic insights into decongestion and diuretic response were lacking, such as analysis of urinary electrolytes and tubular function/damage markers. The study offers the initial evidence for SGLT-2i use in AHF. Although cardiovascular outcome data are lacking in the present study, they provide the foundation to advance further research with SGLT-2i in AHF. Similar success was also achieved with empagliflozin in early post-myocardial infarction (MI) phase in the EMMY trial.4 The use of empagliflozin led to better NT-pro-BNP reduction and high left ventricular EF improvement in 476 patients with post-MI without any safety signals. Two ongoing trials namely EMPA-AHF trial5 and EMPA-RESPONSE-AHF trial6 will further refine the role of empagliflozin in patients with AHF. Hence, despite the seemingly positive results of the EMPULSE study, it will be prudent to wait and watch for results of further trials and may be a follow-up study of EMPULSE before we routinely use SGLT-2 inhibitor therapy in AHF.
Comments (0)